Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Frailty is a syndrome characterized by an increased vulnerability to stressors. Frailty and pre-frailty have been reported in 10% and 44%of community dwelling elderly, respectively.1 Chronic inflammation is a risk factor for frailty. Patients with PMR represent a population at high risk for frailty; however, there are no data on the prevalence and impact of frailty in PMR patients. The objective of this study is to describe the prevalence of frailty in a single center cohort of patients with PMR and to determine the association of frailty with health-related quality of life (HRQoL), cognition and sarcopenia.
Methods: Patients with an ICD-10 diagnosis of PMR were identified between 03/2019-03/2020. Patients fulfilling 2012 EULAR/ACR Provisional Classification Criteria, ≤ 12 months from diagnosis and on glucocorticoids (≥ 3 mg of prednisone) were included. Disease activity was measured with the PMR-activity score. Frailty and pre-frailty were defined according to Fried Frailty Criteria2. HRQoL was assessed using global Patient-Reported Outcomes Measurement Information System (PROMIS) computerized adaptive tests where 50 is the population mean. Cognition was assessed using the Mini-Mental Standard Examination (MMSE) and sarcopenia was assessed by DXA3. Fisher’s exact test, chi-square tests and Kruskal-Wallis tests were used to describe differences among groups as appropriate. Univariate and multivariate linear regressions were used to describe the associations with frailty.
Results: 40 patients were enrolled. Overall, patients had a low burden of comorbidities and high education level (Table 1). Prevalence of frailty, pre-frailty and robustness was 15%,60% and 25%, respectively. Frail patients were older and had longer duration of disease; however, these differences were not statistically significant. Of 27 patients with body composition analysis, 26% were sarcopenic. Frail patients had worse physical function (lower scores) and more fatigue, pain behavior and interference (higher scores) compared to pre-frail and robust patients (Table 2). In the multivariate analysis, frail patients were more likely to have worse physical function, more fatigue, and more pain behavior and pain interference. No significant associations between either cognition or sarcopenia and frailty were observed.
Conclusion: In this cohort of PMR patients, we found a higher prevalence of frailty and pre-frailty than community dwelling elderly. Frailty was associated with worse physical function and increased fatigue, pain behavior and pain interference, differences that were clinically meaningful and statistically significant. Study limitations include the relatively small, homogenous sample size and missing data regarding sarcopenia. These data suggest that frailty is common in PMR and that it is associated with clinical phenotypes. Further assessment of frailty and its impact on PMR outcomes in a larger prospective cohort is warranted.
References
- Collard RM et al. 2012
- Bandeen-Roche et al. 2006
- Cruz-Jentoftet al. 2019
 Figure 1. Fried Frailty Classification
Figure 1. Fried Frailty Classification
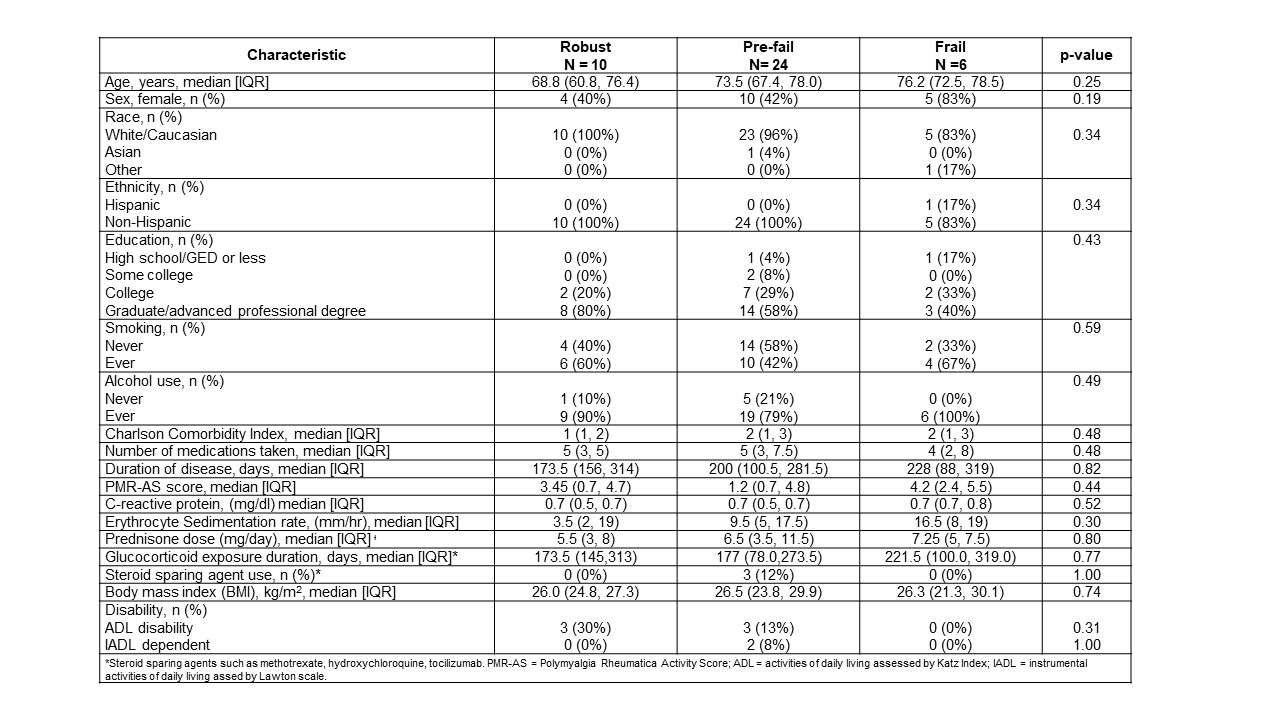 Table 1. Baseline characteristics by frailty classification
Table 1. Baseline characteristics by frailty classification
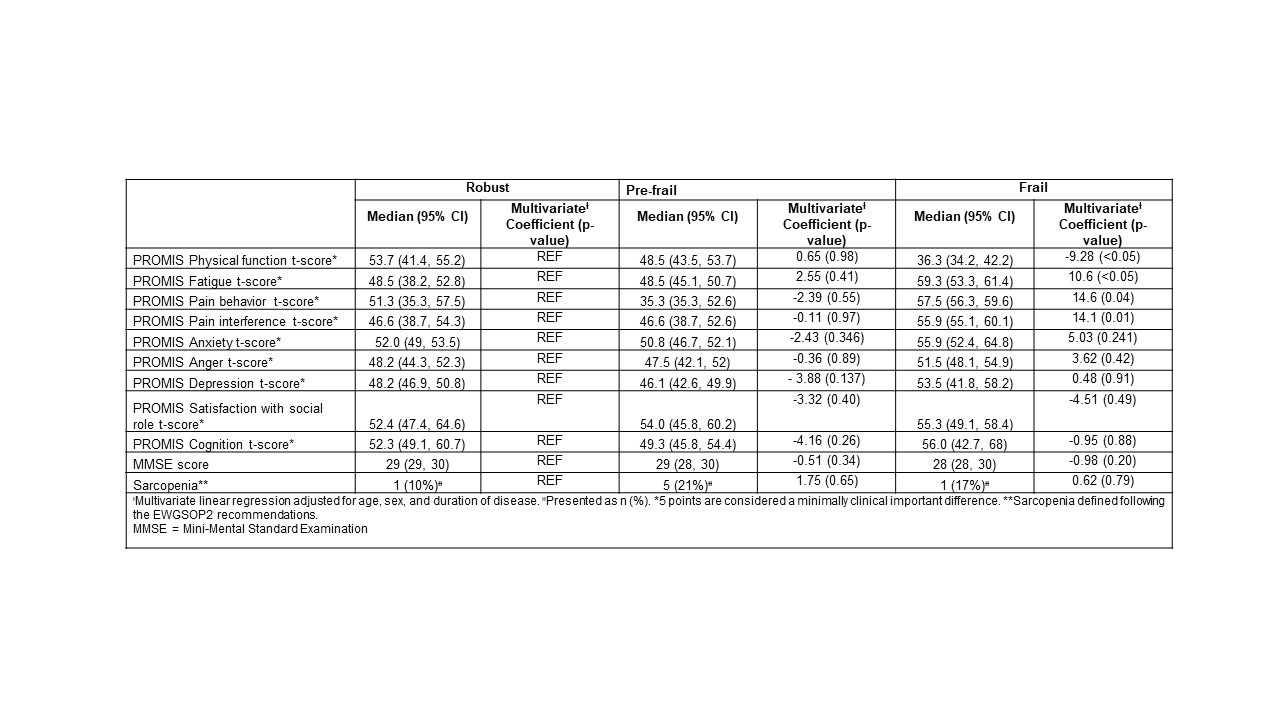 Table 2. HRQoL, MMSE and Sarcopenia by frailty classification and Multivariate Cross-Sectional Analysis
Table 2. HRQoL, MMSE and Sarcopenia by frailty classification and Multivariate Cross-Sectional Analysis
To cite this abstract in AMA style:
Sattui S, Jannat-Khah D, Lally L, Lieber S, Mandl L, Spiera R. Frailty and Health-Related Quality of Life in Patients with Polymyalgia Rheumatica [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/frailty-and-health-related-quality-of-life-in-patients-with-polymyalgia-rheumatica/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frailty-and-health-related-quality-of-life-in-patients-with-polymyalgia-rheumatica/
