Session Information
Date: Monday, November 8, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Outcomes (1257–1303)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Omega-3 fatty acid-derived “specialized pro-resolving mediators” (SPM) are low-abundance lipid mediators (LM) central to inflammation resolution. In this cross-sectional study, we investigated whether fish oil (FO) supplementation was associated with pro-inflammatory and pro-resolving LM in SLE patients compared to matched non-SLE controls.
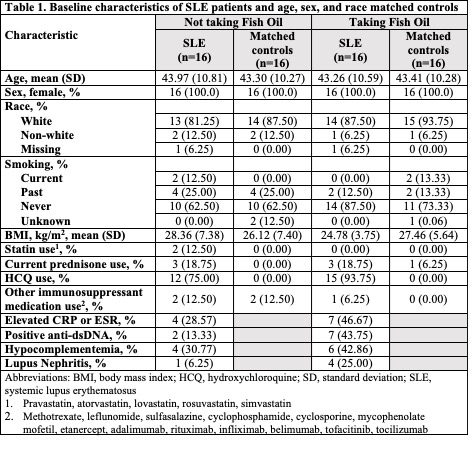
Methods: Within the Mass General Brigham Biobank, we identified 16 patients with SLE taking FO, who were matched by age, sex, and race to 16 patients without SLE taking FO. Another 16 patients with SLE not taking FO were matched on the same factors to 16 non-SLE patients not taking FO. Demographic and clinical data were obtained by medical record review (Table 1). Targeted liquid chromatography-tandem spectroscopy was performed on plasma to quantify 27 omega-3-derived LM, identified with >6 diagnostic ions by tandem mass spectrometry (MS-MS). Multivariable linear analyses examined whether SLE, FO, and the interaction between SLE and FO were associated with LM levels (log-transformed to improve normality), adjusting for smoking status, body mass index and medications. In SLE case-only analyses, we additionally adjusted for C-reactive protein or erythrocyte sedimentation rate (normal/elevated), anti-double stranded DNA (dsDNA positive/negative), C3 and C4 (normal/low), and presence of lupus nephritis. We adjusted for multiple comparisons using a False Discovery Rate (FDR) with a cut-off of 0.05. For missing data, we used multiple imputation.
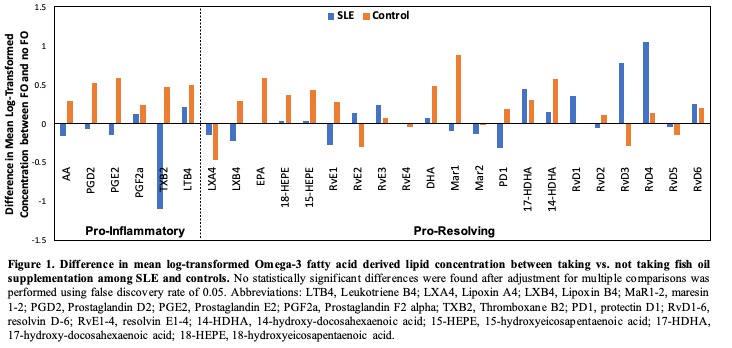
Results: Among SLE patients, lower levels of arachidonic acid (AA) and most (60%) of its pro-inflammatory derivatives were observed in those taking vs. not taking FO, whereas, among the controls, higher levels of AA and all of its pro-inflammatory derivatives were observed in those taking vs. not taking FO (Figure 1). However, after adjustment for multiple comparisons, there were no significant differences for any LM between SLE compared to matched controls, taking or not taking FO. Among controls, taking FO was associated with higher levels of eicosapentaenoic acid (adjusted ß coefficient 0.67 (95% CI: 0.28-1.07), FDR = 0.04) (Table 2). Taking FO was not associated with SPM levels among SLE patients even after adjusting for markers of disease activity. The interaction between SLE and FO was not statistically significant.
Conclusion: In this cross-sectional study, FO supplementation among SLE patients was not significantly associated with higher levels of several pro-resolving SPMs. This may be related to a higher level of inflammatory burden in SLE patients at baseline, reduced ability to biosynthesize SPMs, or failure to take regular and adequate doses of FO. As FO preparations and doses were not controlled in this observational study, further larger controlled studies should pursue these observations.
To cite this abstract in AMA style:
Choi M, Cook N, Stevens E, Gomelskaya N, Kotler G, Manson J, Lasky-Su J, Tatituri R, Mora S, Lee I, Serhan C, Costenbader K. Fish Oil Supplementation and Pro-inflammatory and Pro-Resolving Lipid Mediators in Patients with and Without Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/fish-oil-supplementation-and-pro-inflammatory-and-pro-resolving-lipid-mediators-in-patients-with-and-without-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/fish-oil-supplementation-and-pro-inflammatory-and-pro-resolving-lipid-mediators-in-patients-with-and-without-systemic-lupus-erythematosus/