Session Information
Date: Monday, November 14, 2022
Title: Metabolic and Crystal Arthropathies – Basic and Clinical Science Poster
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Patients with gout often seek care for painful flares and nearly one-third are prescribed opioids during acute ambulatory visits. Unfortunately, opioids do not address the pathologic mechanisms centrally involved gout, either by lowering serum urate (SU) or reducing acute inflammation, and it is possible that opioid therapy for flare and/or chronic pain from advanced gout could serve as a gateway to chronic opioid use. The purpose of our study was to identify factors associated with prevalent and incident opioid use among gout patients in the Veteran’s Health Administration (VHA) population.
Methods: We performed a retrospective cohort study, identifying patients with gout using national VHA data from 1/1999-9/2015 based on the presence of ≥2 ICD-9 for gout (274.X) (Helget LN et al. Arthritis Care Res 2020). Baseline opioid use was defined as receipt of an opioid in the year prior to the index date (date fulfilling gout algorithm). Associations of baseline characteristics with prevalent opioid use were analyzed using multivariable logistic regression. Among those without prevalent opioid use at baseline, a time-to-event analysis using multivariable Cox proportional hazard models was done to examine associations between patient factors and incident opioid receipt after gout diagnosis. Patients were followed from index date until first opioid receipt with censoring due to death or end of the study period. Factors examined as potential determinants of prevalent and incident opioid use included age, sex, race/ethnicity (acknowledging this as a marker for numerous societal factors), comorbidities, body mass index (BMI), and use of urate-lowering therapy (ULT). Rheumatology encounter (≥ 1 visit up to 1 year prior to index date) and urban/rural residence were also included in models examining incident use.
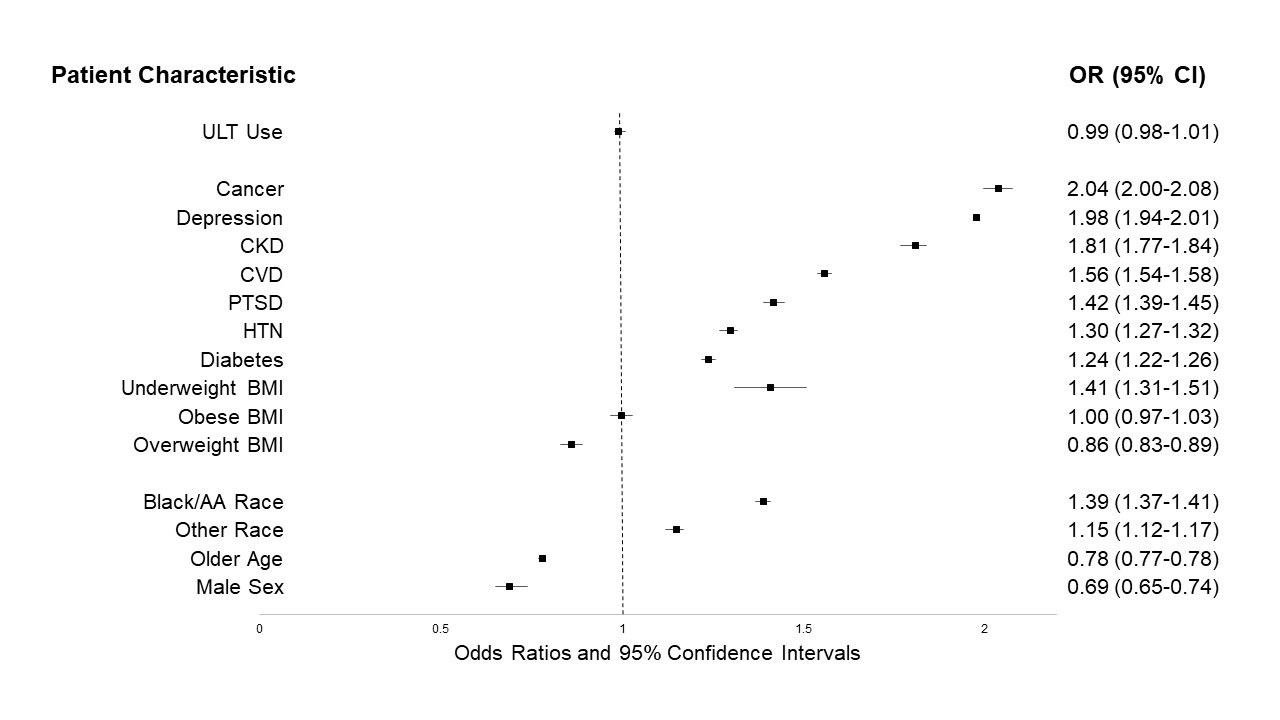
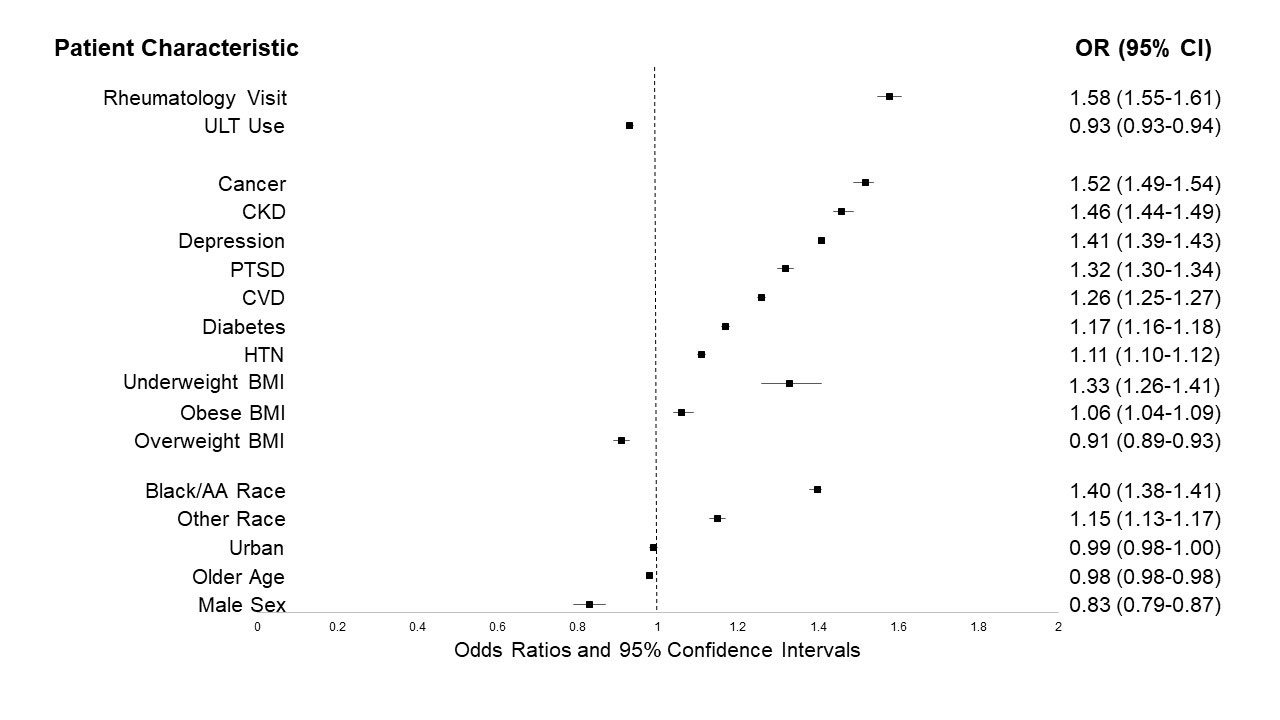
Results: We identified 559,243 gout patients, 25% of whom had prevalent opioid use at the index date. Of 426,564 gout patients without prevalent use at baseline, 44% were prescribed an opioid over a mean follow-up period of 5.5 years (incidence 7.9 per 100 patient-years). Factors associated with prevalent opioid use were younger age, female gender, non-White race, comorbidities, and underweight BMI (Figure 1). Associations of these same factors were similar in analyses of incident opioid use (Figure 2). In models of incident use, a rheumatology encounter was associated with increased risk of opioid use (aHR 1.58; 95% CI 1.55, 1.61) while urban/rural residence showed no association.
Conclusion: Using data from the largest integrated health system in the US, we found nearly 60% of gout patients receive an opioid at some point in time in their disease course. Patient factors including non-white race/ethnicity, comorbidities, and underweight BMI were associated with increased odds of opioid use at baseline as well as incident opioid use over time. Association of incident opioid use with rheumatology care may relate to a referral bias of more severe gout. Additional investigation is needed to understand determinants of opioid use (including chronic use) in gout patients to reduce opioid exposure in this at-risk population.
* All variables included in multivariable model are shown in the figure; white/Caucasian race and normal BMI (20_24.9 km/m2) were referent values; underweight BMI defined as <20 km/m2; overweight BMI defined as 25.0_29.9 km/m2; obese BMI defined as ≥30 km/m2; Other race includes composite of Asian, Native Hawaiian/Pacific Islander, and American Indian
Abbreviations: urate lowering therapy (ULT), chronic kidney disease (CKD), cardiovascular disease (CVD), post-traumatic stress disorder (PTSD), hypertension (HTN), body mass index (BMI), African American (AA)
* All variables included in multivariable model are shown in the figure; white/Caucasian race and normal BMI (20_24.9 km/m2) were referent values; underweight BMI defined as <20 km/m2; overweight BMI defined as 25.0_29.9 km/m2; obese BMI defined as ≥30 km/m2; Other race includes composite of Asian, Native Hawaiian/Pacific Islander, and American Indian
Abbreviations: urate lowering therapy (ULT), chronic kidney disease (CKD), cardiovascular disease (CVD), post-traumatic stress disorder (PTSD), hypertension (HTN), body mass index (BMI), African American (AA)
To cite this abstract in AMA style:
Helget L, England B, Roul P, Sayles H, Petro A, Neogi T, O'Dell J, Mikuls T. Factors Driving Opioid Use in United States Veterans with Gout [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/factors-driving-opioid-use-in-united-states-veterans-with-gout/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-driving-opioid-use-in-united-states-veterans-with-gout/