Session Information
Date: Sunday, November 8, 2020
Title: RA – Diagnosis, Manifestations, & Outcomes Poster III: Cardiopulmonary Aspects
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Heart failure (HF) is a major cause of mortality in rheumatoid arthritis (RA) and is broadly categorized into two subtypes, each with distinct pathophysiology: HF with preserved ejection fraction (HFpEF) and HF with reduced EF (HFrEF). Studies of HF subtypes in RA are limited as the EF data are typically embedded in narrative notes. Natural language processing (NLP) has allowed for efficient extraction of EF data from the electronic health records (EHR) facilitating studies of HF subtypes. The objective of this study was to examine the association between clinical risk factors for incident HF as well as the two subtypes, HFpEF and HFrEF, among RA patients.
Methods: Utilizing a validated EHR-based RA cohort (n=16,248), we identified patients with HF using a published approach (PPV=90%) and extracted EF using NLP from cardiac imaging reports. The RA index date was defined as the first occurrence of RA ICD-9, 10, or NLP code. The HF incident date was the date of the first HF ICD code. patients with HF were classified into HFrEF (EF< 40%) or HFpEF (EF >50%) using the EF value closest to the HF incident date. We excluded patients with < 1-year of EHR data, and those with HF prior to the RA index date. Follow-up started at the RA index date and continued through incident HF or a censoring event (death or last known visit date). Demographics were assessed at the RA index date; known comorbidities associated with HF from the general population were assessed from EHR entry to RA index date; and RA-specific factors were assessed from the RA index date until HF diagnosis or censoring; erythrocyte sedimentation rate (ESR), the most common inflammatory marker available was averaged from RA index date to either HF event or time of censoring. We tested the association between RA-specific factors with overall HF, HFpEF, and HFrEF using logistic regression adjusting for potential confounders.
Results: We studied 8635 RA patients of which 1007 (11.7%) developed HF during 9.3 (SD 6.5) years follow-up. In this RA cohort, patients with HF were older, more likely to be male, Caucasian, and had more comorbidities compared to those without HF (Table 1).
Higher levels of ESR was associated with a higher overall HF risk and across both subtypes compared to RA patients without HF, while MTX use was associated with a reduced risk in all HF patients, and in HFpEF and HFrEF (Table 2). TNFi and nbDMARD use was associated with a reduced risk of HFpEF but not HFrEF, after adjusting for potential confounders. Comorbidities more strongly associated with HFpEF and not HFrEF included valvular disease, hypertension, and diabetes, consistent with studies from the general population.
Conclusion: In this large cohort of RA patients, we observed differences in risk factors associated with incident HFpEF compared to HFrEF. While TNFi use is not recommended for patients with moderate to severe HF, these data suggest that TNFi’s may have a different effect for risk of HF depending on the subtype. Future studies with more detailed drug data are needed to closely examine DMARD use and risk of HFpEF vs HFrEF in RA.
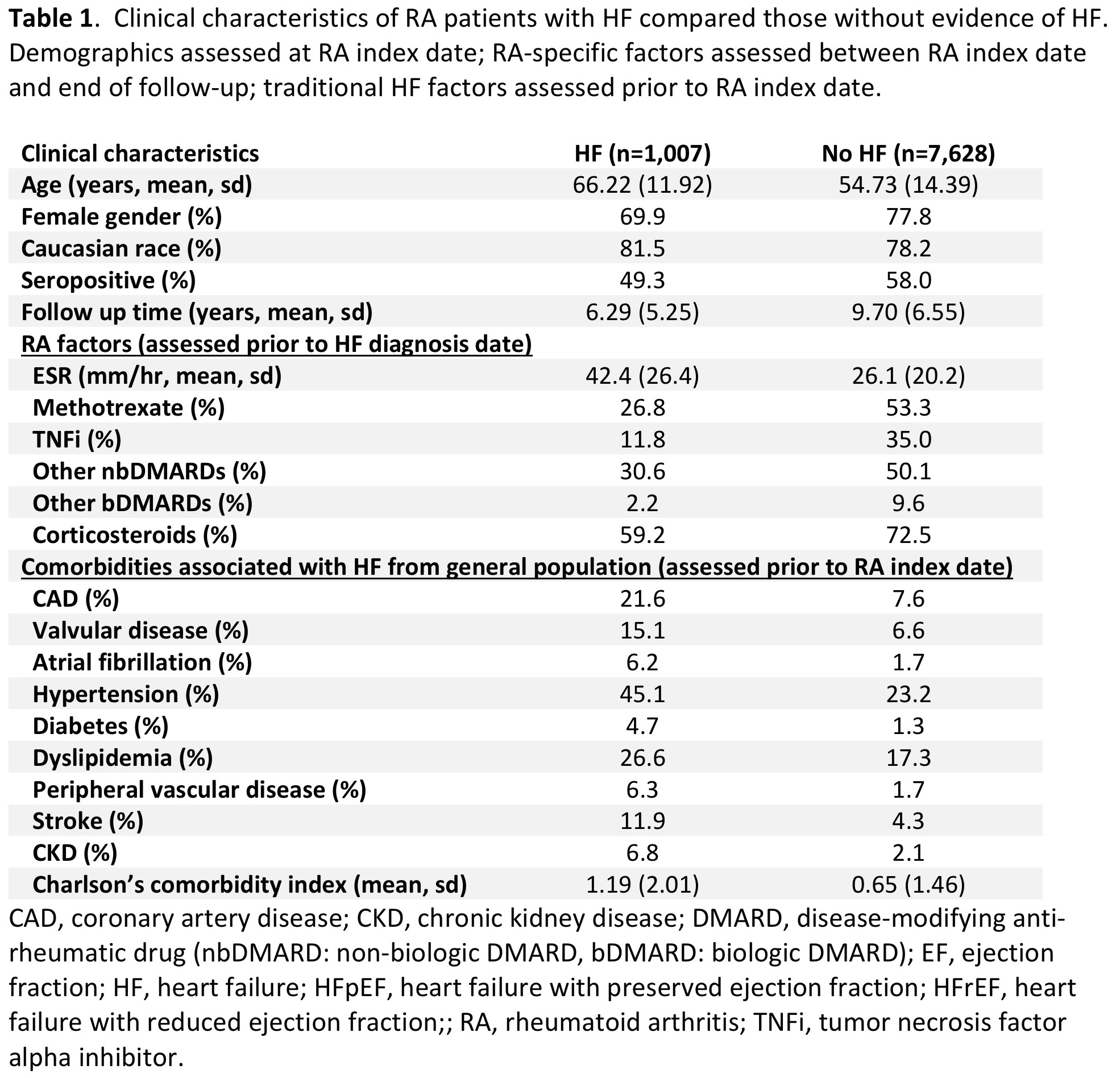 Table 1. Clinical characteristics of RA patients with HF compared those without evidence of HF.
Table 1. Clinical characteristics of RA patients with HF compared those without evidence of HF.
 Table 2. Clinical factors associated with incident (a) HF, (b) HFpEF, and (c) HFrEF vs. no HF (reference) among RA patients.
Table 2. Clinical factors associated with incident (a) HF, (b) HFpEF, and (c) HFrEF vs. no HF (reference) among RA patients.
To cite this abstract in AMA style:
Huang S, Cai T, Weber B, He Z, Dahal K, Hong C, Cagan A, Joseph J, Kim S, Solomon D, Cai T, Liao K. Factors Associated with Incident Heart Failure Subtypes in Patients with Rheumatoid Arthritis Using Electronic Health Record Data [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/factors-associated-with-incident-heart-failure-subtypes-in-patients-with-rheumatoid-arthritis-using-electronic-health-record-data/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-incident-heart-failure-subtypes-in-patients-with-rheumatoid-arthritis-using-electronic-health-record-data/
