Session Information
Date: Tuesday, November 12, 2019
Title: RA – Diagnosis, Manifestations, & Outcomes Poster III: Comorbidities
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: For patients with rheumatoid arthritis (RA), heart failure (HF) is a significant cause of morbidity and mortality. HF is further classified into 2 subtypes to guide management; HF with preserved ejection fraction (HFpEF) and HF with reduced ejection fraction (HFrEF). HFrEF is commonly observed after myocardial ischemia due to myocyte loss. Chronic inflammation is proposed to play a major role in HFpEF even in the absence of a chronic inflammatory condition. These HF subtypes have been traditionally difficult to study in RA due to the need for a large RA cohort with ejection fraction (EF) data. The objective of this study was to test existing approaches using natural language processing (NLP) to characterize HF subtypes in an electronic medical record (EMR) based RA cohort, and to study differences in clinical risk factors between the two HF subtypes in RA.
Methods: We used data from an EMR-based RA cohort from 2 tertiary care centers. Within this cohort we applied a published protocol using machine learning and natural language processing (NLP) to identify patients with HF. Among RA patients with HF, we further applied an NLP tool to extract EF data from cardiology reports. Incident HF cases (RA-HF) were identified and matched 1:3 by age, sex, and healthcare utilization to RA patients without HF. HF was classified using the EF data into HFrEF (EF< 40%) and HFpEF (EF >50%). The index date for HF patients was the date of the first EF measurement; thus, this study was limited to HF patients with EF in their records. For controls, the index date was the closest healthcare utilization date within a 6-month window for the EF date. We assessed covariates including RA clinical factors and traditional HF risk factors over the 3-year period prior to the index date. Using a case-control design, conditional logistic regression was performed to identify risk factors associated with the development of unclassified HF, HFpEF, and HFrEF.
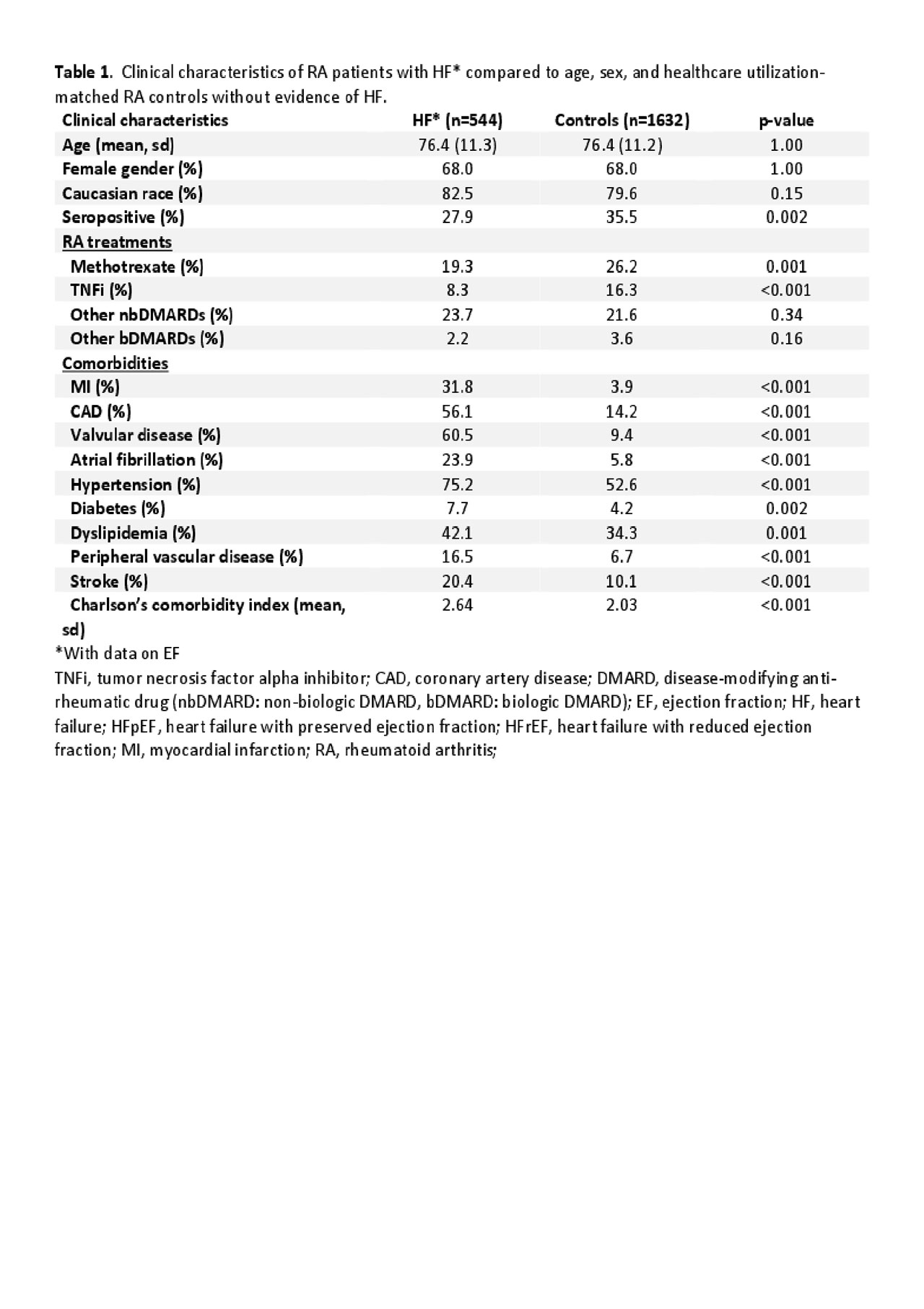
Results: We identified 544 RA subjects with incident HF and EF data. Compared to age and sex matched controls, the RA-HF subjects were less likely to be seropositive or on methotrexate or TNF-α inhibitor (TNFi), and have more comorbid conditions (Table 1). Among RA clinical factors, methotrexate was associated with a lower risk of any HF and HFpEF, and not HFrEF. TNFi use was also associated with reduced risk of any HF, with a stronger trend for reduction in HFpEF (Table 2). Traditional HF risk factors such as myocardial infarction (MI) and coronary artery disease (CAD) were associated with increased risk of any type of HF, with stronger association with HFrEF; valvular disease and atrial fibrillation were more strongly associated with increased risk for HFpEF, consistent with prior literature.
Conclusion: In this preliminary study, we observed that RA factors such as MTX and TNFi use was associated with reduced risk of HF, specifically HFpEF in the former. These differences may provide guidance on understanding the role of inflammation and HFpEF in RA, where anti-inflammatory therapies may provide benefit. Future work is needed to validate incident HF and EF definitions and to take into account the time-varying effect of DMARDs and disease activity on the risk of HF and its subtypes in RA.
To cite this abstract in AMA style:
Huang S, Cai T, Solomon D, He Z, Dahal K, Hong C, Cagan A, Kim S, Joseph J, Cai T, Liao K. Factors Associated with Differing Types of Heart Failure in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/factors-associated-with-differing-types-of-heart-failure-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-differing-types-of-heart-failure-in-patients-with-rheumatoid-arthritis/