Session Information
Date: Tuesday, November 9, 2021
Title: Patient Outcomes, Preferences, & Attitudes Poster IV: COVID-19 (1589–1613)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: COVID-19 vaccination efforts are ongoing and there is a need to understand factors associated with vaccine hesitancy. Individuals with rheumatic diseases have been uniquely impacted by the COVID-19 pandemic and little is known about vaccine acceptance rates in this population in the United States. The objective of this study was to identify reasons for vaccine hesitancy as well as associated risk factors in a US-based rheumatic disease population.
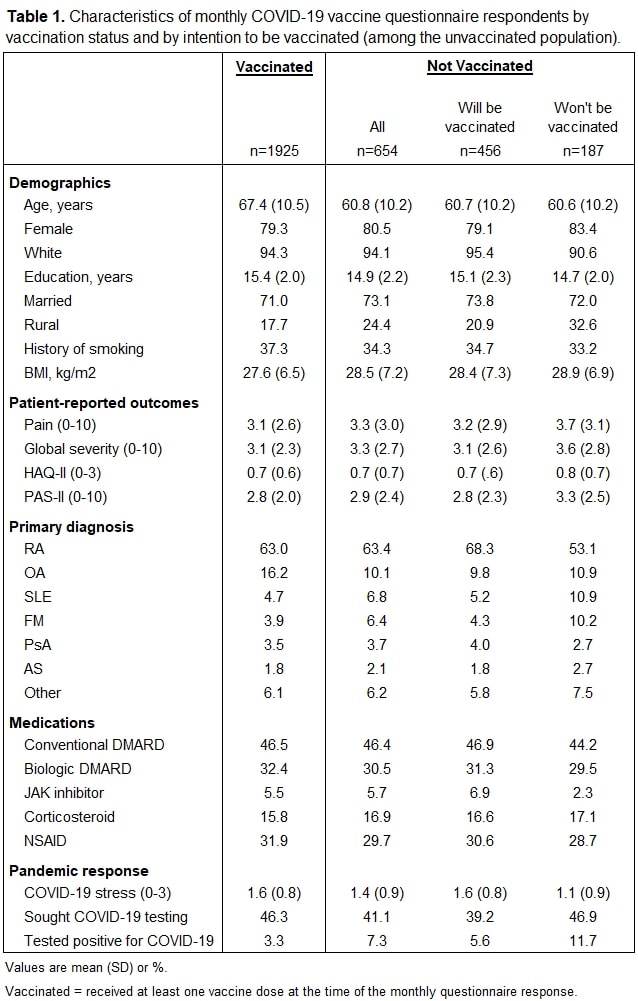
Methods: Data were provided by adults enrolled in FORWARD, The National Databank for Rheumatic Diseases. Participants complete comprehensive semiannual questionnaires and were invited to answer supplemental questionnaires focused on COVID-19 vaccination in March and April 2021. Responses to the supplemental questionnaires were linked to each participant’s most recently completed semiannual questionnaire for demographics, diagnosis, patient-reported outcome measures, medication use, and pandemic response variables. Respondents were compared by vaccination status, and (among those who were unvaccinated) by intention to be vaccinated. Reported reasons for vaccine hesitancy were described for those respondents who did not intend to be vaccinated, and risk factors associated with vaccine hesitancy were identified with logistic regression adjusted for age, sex, race, education, rural residency, BMI, physical function (HAQ-II), COVID-19-specific stress (Likert scale), and diagnosis (RA reference).
Results: Among the 2,579 unique respondents, 1,925 (75%) reported receiving at least one dose of a COVID-19 vaccine at the time of questionnaire completion. Of those who were not vaccinated, 456 (71%) reported an intention to be vaccinated in the future (Table 1). Of those who did not plan to receive a COVID-19 vaccine (n=187, 7% of respondents), the most frequently reported reason was concern about side effects (54%), followed by distrust (47%), and concern about sufficient testing on individuals with rheumatic diseases (40%; Figure 1A). Many respondents selected multiple reasons for vaccine hesitancy, and the most frequently reported groups of responses are ranked in Figure 1B. Respondents of non-white race were significantly more likely to be vaccine hesitant (OR [95% CI] = 6.7 [2.0, 22]; p=0.002), as were individuals with higher HAQ-II scores (1.8 [1.1, 2.9]; p=0.024; Figure 2). Respondents with a primary diagnosis of SLE were significantly more likely to be vaccine hesitant than were individuals with RA (2.7 [1.1, 7.1]; p=0.038). Individuals who reported higher levels of pandemic-related stress were significantly less likely to be vaccine hesitant (0.4 [0.3, 0.6]; p< 0.001).
Conclusion: Most individuals in this cohort had already been vaccinated against COVID-19 or intended to be vaccinated. The difference in vaccine hesitancy by race is consistent with reports on vaccine hesitancy in populations not specific to individuals with rheumatic diseases. Most of the frequently reported reasons for vaccine hesitancy were related to concerns about possible physical responses to COVID-19 vaccines or to perceived lack of information/knowledge, both of which could potentially be addressed by education from a health care provider.
To cite this abstract in AMA style:
Wipfler K, Cornish A, Freifeld A, Katz P, Michaud K. Factors Associated with COVID-19 Vaccine Hesitancy Among Individuals with Rheumatic Disease [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/factors-associated-with-covid-19-vaccine-hesitancy-among-individuals-with-rheumatic-disease/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-covid-19-vaccine-hesitancy-among-individuals-with-rheumatic-disease/