Session Information
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: SLE disproportionately affects patients of color. Medication nonadherence is more common among patients of color with SLE and is associated with worse health outcomes. We aimed to better understand factors that make adherence to immunosuppressive medications easier among patients of color with SLE.
Methods: Using a qualitative descriptive study design, we conducted in-depth interviews with purposefully selected samples of 1) lupus clinic providers and staff, and 2) patients of color with SLE taking immunosuppressants (MTX, AZA, or MMF) from an academic lupus clinic. We asked participants about adherence facilitators. We probed patients on approaches to overcome common adherence challenges and providers and staff on actions they can take to enable adherence. We audio-recorded and transcribed interviews verbatim and analyzed them using applied thematic analysis. We categorized themes using the Capability, Opportunity, Motivation, Behavior conceptual model. In this model, Capability refers to external factors that help patients acquire medications; Opportunity corresponds to factors that enable adherence on a regular basis; and Motivation corresponds to factors that affect conscious and unconscious beliefs and attitudes.
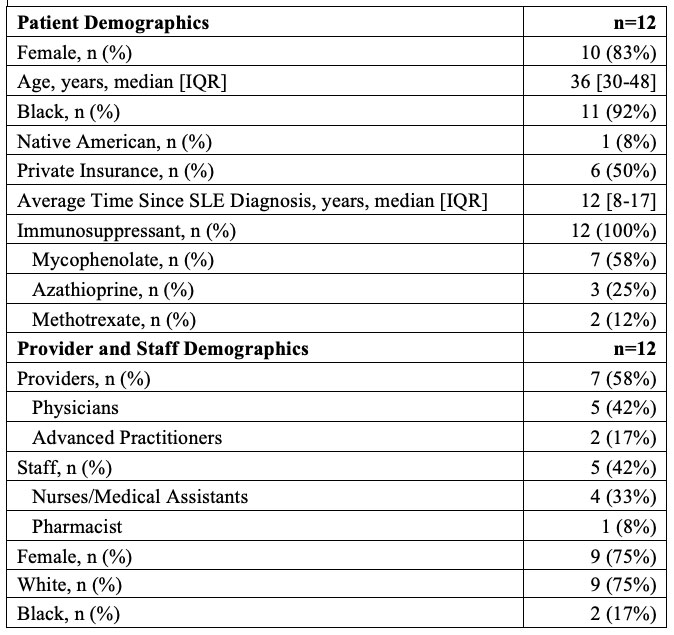
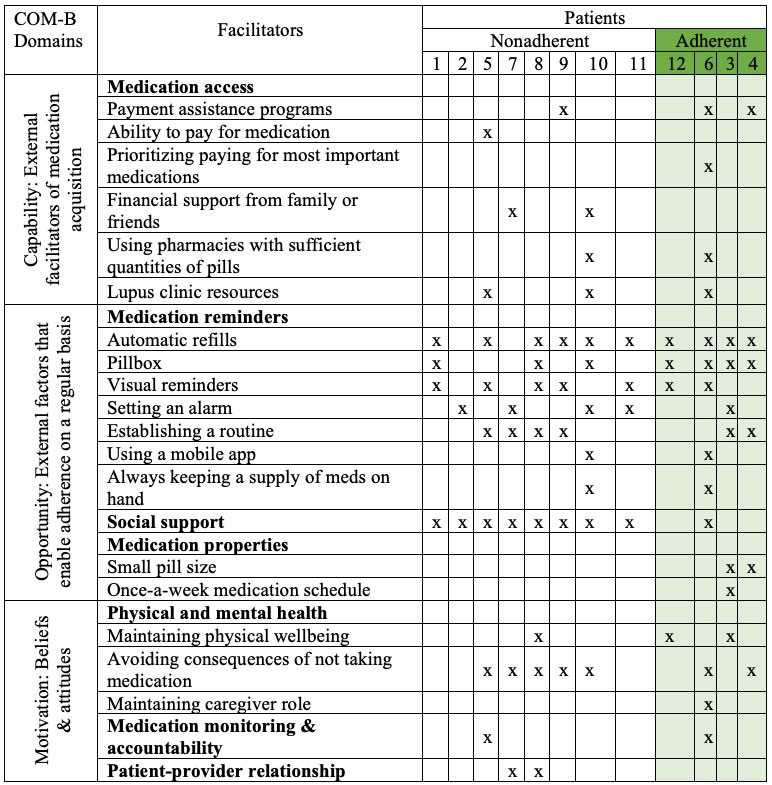
Results: We interviewed 12 providers and staff (7 providers, 5 staff) and 12 patients (4 adherent, 8 nonadherent). Participant characteristics are summarized in Table 1. The most described facilitators among patients were social support, notable health benefits, reminders, and ability to acquire medications. The latter two were also commonly described by providers and staff, who additionally focused on patient education and communication, and empowerment and acceptance. Remaining facilitators identified included medication properties such as pill size and dosing schedule, medication monitoring and accountability, and patient-provider relationship (Table 2).
Each patient described a unique set of facilitators spanning the three behavioral domains. Although most facilitators were described similarly by both adherent and nonadherent patients, pillboxes were identified by all adherent patients but only half of nonadherent patients. Similarly, medication properties were solely identified by adherent patients as a facilitator. Conversely, social support was described by all nonadherent patients and only a quarter of adherent patients as a facilitator.
Conclusion: Our results suggest that the optimal intervention to improve medication adherence will likely require a multi-modal and individually tailored approach including components from each behavioral domain—ensuring medication access (Capability), utilizing reminders and social support (Opportunity), coupled with internal motivation through patient education and empowerment (Motivation). While some interventions (e.g., medication reminders) can be easily implemented, others (e.g., medication properties and access, and patient education) will likely require organizational and societal changes, highlighting the resources needed to serve the needs of patients with SLE, particularly those from disadvantaged backgrounds.
To cite this abstract in AMA style:
Herndon S, Corneli A, Dombeck C, Swezey T, Clowse M, Rogers J, Criscione-Schreiber L, Sadun R, Doss J, Eudy A, Bosworth H, Sun K. Facilitators of Immunosuppressive Medication Adherence in Systemic Lupus Erythematosus: A Qualitative Study of Racial Minority Patients, Lupus Providers and Clinic Staff [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/facilitators-of-immunosuppressive-medication-adherence-in-systemic-lupus-erythematosus-a-qualitative-study-of-racial-minority-patients-lupus-providers-and-clinic-staff/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/facilitators-of-immunosuppressive-medication-adherence-in-systemic-lupus-erythematosus-a-qualitative-study-of-racial-minority-patients-lupus-providers-and-clinic-staff/