Session Information
Date: Monday, November 14, 2016
Title: Systemic Sclerosis, Fibrosing Syndromes, and Raynaud's – Clinical Aspects and Therapeutics II
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Prognostication in scleroderma has historically depended on using static measures such as antibody status and extent of skin involvement to stratify risk of mortality and major organ complications. These static measures are intrinsically unable to inform the difference between disease activity and disease damage in scleroderma, which is a critical for clinicians considering the timing of potentially toxic treatment. We hypothesized that serial changes in a clinical outcome of interest–in this case the forced vital capacity (FVC)Ñcould itself be used to classify patients with a common disease course and comparable mortality.
Methods: We retrospectively applied a form of latent subtype analysis called probabilistic subtype modeling (PSM) to serial lung function data from patients followed at an academic scleroderma referral center, to identify shared trajectories of FVC among individuals over time. We then examined mortality across each of these shared trajectories using Kaplan Meier curves and adjustment for demographics with Cox proportional hazards models.
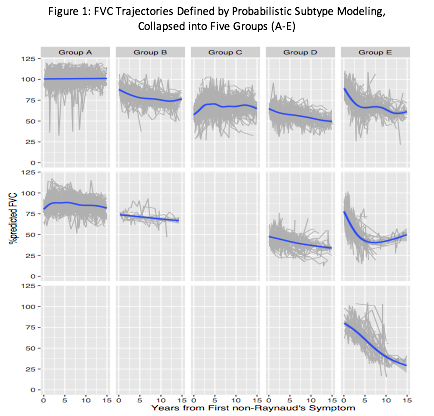
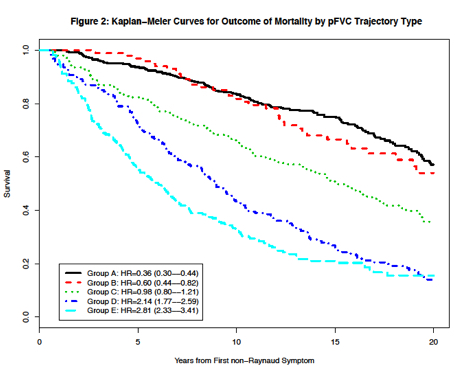
Results: Serial FVC from 1615 patients defined 10 trajectories by PSM, which were collapsed by the authors into 5 clinically similar patterns of FVC change over time (Figure 1). Mortality separated largely into 3 groups (Figure 2), with a protective hazard in subgroups with intact lung function (HR of 0.36 [95%CI=0.30Ñ0.44] and 0.60 [0.44Ñ0.82]) in Groups A and B, respectively, an intermediate mortality in the subgroup with variable FVC (Group C HR 0.98 [0.80Ñ1.21]), and a high mortality among patients with depressed and declining FVC (HR 2.14 [1.77Ñ2.59] and 2.81 [2.33Ñ3.41] in Groups D and E, respectively). Major antibody, skin extent, race, gender, disease onset after age 55, and the presence of calcinosis most frequently helped distinguish among the FVC trajectory subtypes. However, the highest prevalence of any single characteristic within a subtypeÑfor example, diffuse skin (68%) or centromere antibody (37%)Ñwere not sufficiently associated with an FVC trajectory to serve as the only distinguishing feature among subtypes.
Conclusion: Grouping patients by longitudinal change in FVC identifies patients with similar risk of mortality, illustrating the potential utility of incorporating serial clinical metrics into the risk assessment of patients with scleroderma. If identifiable early within an individualÕs course, clinical trajectories may be powerful tool to inform treatment decisions.
To cite this abstract in AMA style:
Ligon C, Schulam P, Saria S, Wigley FM, Wise R, Hummers LK. Faces in Motion: Clinical Subtyping in Scleroderma Using Changes in Forced Vital Capacity [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/faces-in-motion-clinical-subtyping-in-scleroderma-using-changes-in-forced-vital-capacity/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/faces-in-motion-clinical-subtyping-in-scleroderma-using-changes-in-forced-vital-capacity/