Session Information
Date: Friday, November 6, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Clinical Manifestations
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Using data from the Systemic Lupus International Collaborating Clinics (SLICC) inception cohort, a frailty index (FI) was recently developed as a measure of susceptibility to adverse health outcomes among individuals with SLE. In this work, higher baseline SLICC-FI values were associated with increased organ damage accrual and mortality risk during follow-up. While promising, these results require external validation. The objective of the current study was to evaluate the properties of the SLICC-FI in a prevalent cohort of individuals with more longstanding SLE.
Methods: This was a secondary analysis of data from a prospective cohort of adult SLE patients at a single academic medical center. All participants met the 1997 revised ACR classification criteria for SLE and were assessed annually for medication use, comorbidities, disease activity (SLEDAI-2K), organ damage [SLICC/ACR Damage Index (SDI)], health-related quality of life [Short-Form 36 (SF-36)], and other measures.
For this analysis, we defined the baseline visit as the first visit at which both SDI and SF-36 data were available. We created an adapted version of the original SLICC-FI by modifying the definitions of individual health deficits based on data availability. Using 48 health deficits, we calculated a baseline SLICC-FI score for each patient. Vital status and SDI score at last follow-up were recorded.
Cox regression was used to estimate the association between baseline SLICC-FI values and mortality risk. Negative binomial regression was used to estimate the association of baseline SLICC-FI values with the rate of change in SDI scores per patient-year of follow-up. Multivariable models adjusted for relevant baseline variables.
Results: The 329 eligible SLE patients (96% of cohort) were mostly female (88%) with mean (SD) age 43.9 (14.4) years and median (IQR) disease duration 3.4 (1.2-13.3) years at baseline. Mean (SD) baseline SLICC-FI score was 0.17 (0.08), with 94 patients (28.6%) classified as frail (SLICC-FI > 0.21).
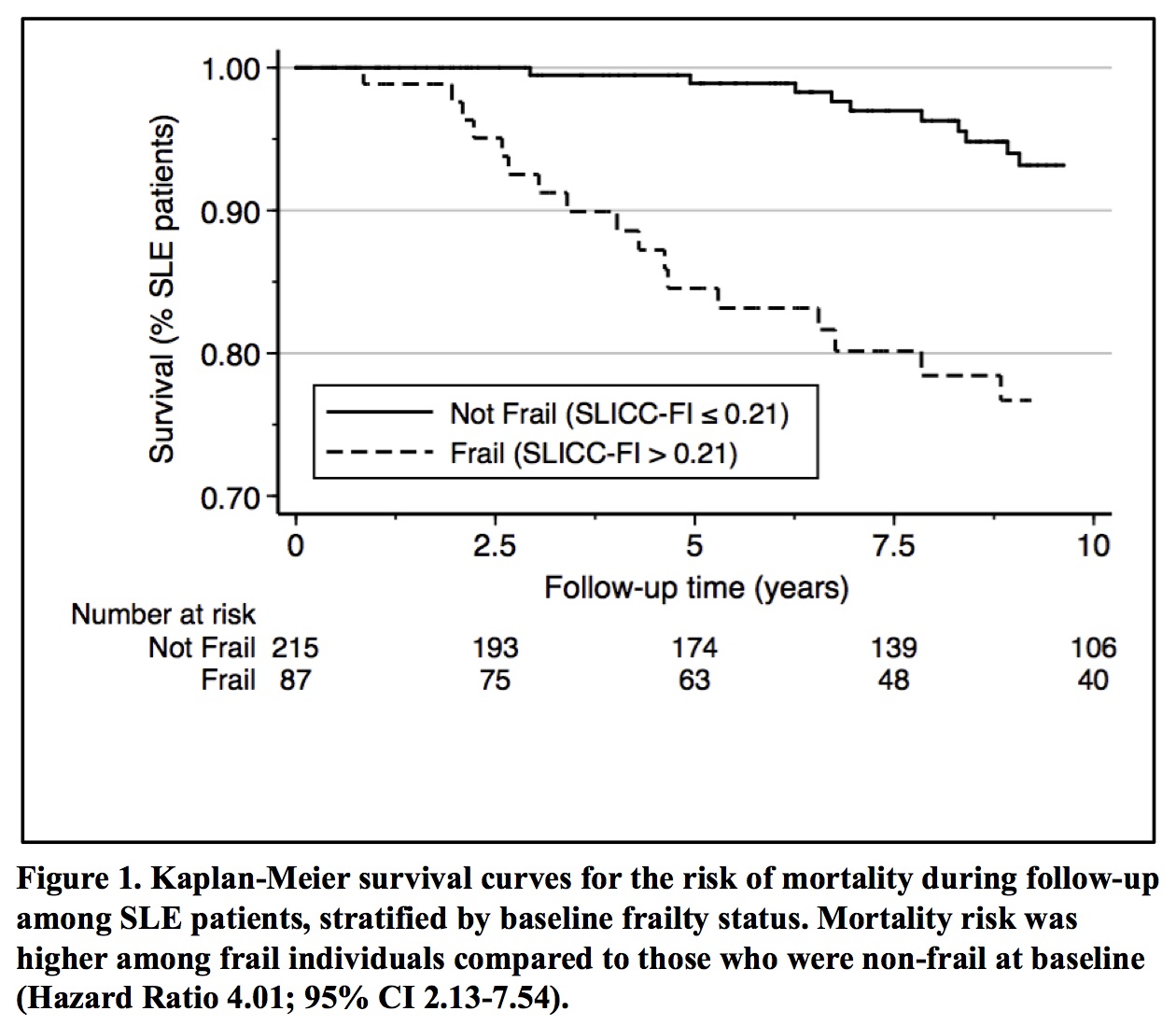
Forty deaths occurred during mean (SD) follow-up of 10 (5.5) years. Mortality risk was significantly higher among frail individuals (Figure 1). Higher baseline SLICC-FI values (per 0.05 units) were associated with increased mortality risk (Hazard Ratio 1.42; 95% CI 1.14-1.78), after adjusting for age, sex, education, SLE medication use, disease duration, smoking status, and baseline SDI (Table 1).
There were 133 patients with an increase in SDI score during follow-up. Higher baseline SLICC-FI values (per 0.05 units) were associated with increased damage accrual over time (Incidence Rate Ratio 1.19; 95% CI 1.09-1.31), after adjusting for age, sex, corticosteroid use, disease duration, smoking status, and baseline SDI (Table 2).
These associations between baseline SLICC-FI values and adverse health outcomes persisted when inception patients (disease duration < 15 months at enrolment) were excluded, and when items related to organ damage were omitted from the SLICC-FI.
Conclusion: Frailty, measured using the SLICC-FI, predicts organ damage accrual and mortality risk among individuals with established SLE. This external validation study provides additional support for the SLICC-FI as a useful prognostic tool in SLE.
To cite this abstract in AMA style:
Malone A, Legge A, Hanly J. External Validation of the Systemic Lupus International Collaborating Clinics Frailty Index (SLICC-FI) as a Predictor of Mortality and Organ Damage Accrual in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/external-validation-of-the-systemic-lupus-international-collaborating-clinics-frailty-index-slicc-fi-as-a-predictor-of-mortality-and-organ-damage-accrual-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/external-validation-of-the-systemic-lupus-international-collaborating-clinics-frailty-index-slicc-fi-as-a-predictor-of-mortality-and-organ-damage-accrual-in-systemic-lupus-erythematosus/