Session Information
Date: Monday, November 14, 2016
Title: Rheumatoid Arthritis – Clinical Aspects - Poster II: Co-morbidities and Complications
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Antihypertensives (antiHT) and lipid lowering therapies (LLT) prevent cardiovascular disease (CVD) effectively. It has been reported that patients with rheumatoid arthritis (RA) receive suboptimal CVD-prevention. Whether other inflammatory joint diseases (IJD), such as ankylosing spondylitis (AS), psoriatic arthritis (PsA) and other spondyloarthropathies (SpA), also receive inadequate CVD management remains unknown. In a large IJD cohort we aimed to evaluate 1) Rate of indications for antiHT and/or LLT, 2) rate of antiHT and/or LLT initiation, and 3) blood pressure (BP) and low-density lipoprotein cholesterol (LDL) goal attainment in patients treated with antiHT or LLT, respectively.
Methods: The present IJD cohort is derived from the Norwegian COllaboration on Cardiovascular disease in patients with Rheumatic joint diseases (NOCAR). In NOCAR, CVD risk factors are collected in daily rheumatology practice. Need for antiHT was defined as BP ≥140/90mmHg or self-reported hypertension (HT). BP levels <140/90 mmHg were recognized as BP goal attainment. Ten year risk of a fatal CVD event was estimated by the Systematic COronary Risk Evaluation (SCORE). According to guidelines, patients with diabetes, hyperlipidemia or SCORE ≥5% are at high CVD risk and should receive LLT (LDL target <2.6 mmol/L); whereas established CVD or SCORE ≥10% imply a very high CVD risk (LDL target <1.8 mmol/L). Rates were calculated for the whole cohort and compared across IJD entities using logistic regression, age and sex adjusted.
Results: Of the 2647 patients (RA: n=1696, AS: n=445, PsA: n=376, SpA: n=130), 53.2% had indication for antiHT, and this was significantly higher in RA (57.0%) and PsA (57.2%). Among patients for whom antiHT was indicated, 59.0% received treatment and half of the patients on antiHT had obtained BP goal. There was indication for LLT in 24.1%, which was comparable across the IJD entities except for AS (14.4%) (p<0.0001). In the group with indication for LLT, 55.6% had high CVD risk which was most frequently seen in PsA (p=0.02), whereas 43.7% had very high CVD risk, which was more common in AS patients (p=0.02). Half of the patients with indication for LLT received this therapy, and treatment rates were higher for patients with very high CVD risk compared to those with high CVD risk (p<0.001). In total, 16.8% had achieved LDL treatment targets; LDL goal attainment was particularly high in PsA patients (p<0.01), and higher in patients with high CVD risk than in those with very high CVD risk (p<0.001). 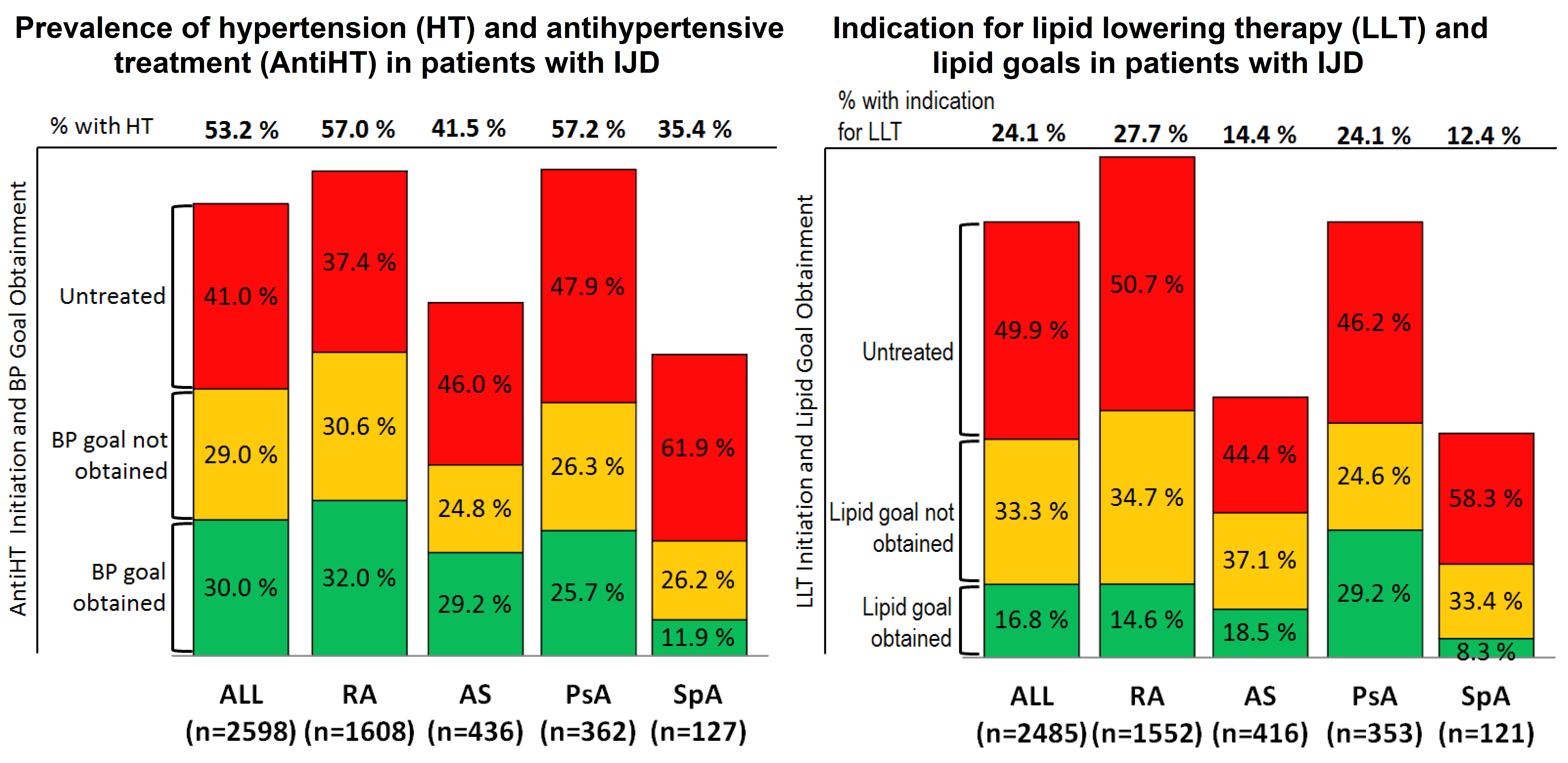
Conclusion: CVD-preventive medication is often indicated, but infrequently initiated in IJD patients. Moreover, when antiHT and LLT are started, quite few patients obtain treatment goals. There is a need for improving CVD risk assessment, initiation of proper CVD-prevention and careful monitoring of target achievements to successfully reduce the excess CVD risk in IJD patients.
To cite this abstract in AMA style:
Ikdahl E, Rollefstad S, Wibetoe G, Salberg A, Soldal DM, Olsen IC, Kvien TK, Semb AG, Haugeberg G. Exploring the Inadequate Cardiovascular Disease Prevention in Inflammatory Joint Diseases: Results from a Nationwide Norwegian Project [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/exploring-the-inadequate-cardiovascular-disease-prevention-in-inflammatory-joint-diseases-results-from-a-nationwide-norwegian-project/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/exploring-the-inadequate-cardiovascular-disease-prevention-in-inflammatory-joint-diseases-results-from-a-nationwide-norwegian-project/
