Session Information
Date: Monday, November 8, 2021
Title: Abstracts: Systemic Sclerosis & Related Disorders – Basic Science (1434–1437)
Session Type: Abstract Session
Session Time: 11:00AM-11:15AM
Background/Purpose: Interstitial lung disease (ILD) is the major cause of morbidity and mortality in systemic sclerosis (SSc), yet there are few biomarkers to identify pathologic immune activation. T cells play a key role in initiating and promoting lung injury in SSc. Recent reports have indicated that circulating PD-1+ CXCR5+ T follicular helper cells (Tfh) and PD-1hi CXCR5– T peripheral helper cells (Tph) are expanded in SSc patients. Tfh and Tph cells are B cell-helper T cells that can display variable expression of ICOS and/or HLA-DR. Here we have evaluated both the frequency and phenotype of PD-1hi cells in the peripheral blood of SSc patients, and assessed association with ILD.
Methods: We immunophenotyped blood T cells using a 39-marker mass cytometry panel. Peripheral blood mononuclear cells were collected from SSc patients (n=82) and age matched non-inflammatory controls (n=18). Patient samples were analyzed in barcoded batches with each one randomized to include both healthy controls and SSc patients with varying lung disease. Data was analyzed by biaxial gating in FlowJo and by FlowSOM dimensional reduction and clustering. Comparisons between SSc patient samples and healthy controls were performed using Mann-Whitney U test with Bonferroni correction. Association between expanded cell population and lung disease metrics was assessed by Spearman correlation.
Results: In this cohort, the frequencies of Tph (PD-1hi CXCR5–) and Tfh (PD-1hi CXCR5+) CD4 T cells were not increased in SSc patients compared to healthy controls. However, tSNE visualization of PD-1hiCXCR5- cells revealed substantial heterogeneity in expression of ICOS and HLA-DR within this subset. A detailed cytometric analysis of expression of the markers in the cytometry panel on these cell subsets identified upregulation of HLA-DR and CD38 expression on PD-1hi CXCR5– cells from SSc patients compared to controls (Bonferroni adjusted p< 0.05) (Figure 1A). Biaxial gating confirmed the significant expansion of a specific CD4 T cell population with a PD-1hi CXCR5– ICOS– HLA-DR+ phenotype, which was significantly increased in SSc patients compared to healthy controls (0.22% vs. 0.12%, p=0.003) (Figure 1B). This subset was also expanded in patients with SSc-ILD when compared with those without ILD (p=0.02) and healthy controls (HC) (p=0.001) (Figure 2A). Further, the frequency of this CD4 T cells was increased in SSc subjects with more severe ILD (p= 0.017). Consistent with this observation, the frequency of PD-1hi CXCR5– ICOS– HLA-DR+ CD4+ cells in SSc patients showed an inverse correlation with multiple metrics of pulmonary function, including forced vital capacity % predicted (FVCpp, r= -0.34, p=.0043), diffusing capacity for carbon monoxide (DLCO, r= -0.25, p=0.038) and forced expiratory volume 1 % predicted (FEV1pp, r=-0.44, p=0.0002) (Figure 2B).
Conclusion: High dimensional CyTOF analysis conducted in this cohort of SSc patients highlighted a specific expanded CD4+ T cell population (PD-1hi CXCR5– HLA-DR+ ICOS–) that is significantly associated with presence and severity of lung disease. Further studies will evaluate whether this marker can predict the rate of decline of lung function in SSc-ILD, a critically needed tool in the care of patients with SSc.
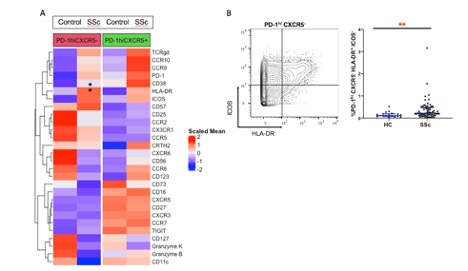 Figure 1. Altered cytometric phenotype of circulating PD_1hi CXCR5- cells in SSc patients. (A) Heatmap of row-normalized expression of cytometry markers on indicated subsets. * indicates markers (HLA-DR, CD38) that are significantly upregulated on PD_1hiCXCR5- cells in SSc compared to controls (Bonferroni adjusted p < 0.05). (B) Biaxial gating of ICOS and HLA-DR expression on PD_1hi CXCR5- memory CD4 T cells. Frequency of PD_1hi CXCR5- HLA-DR+ ICOS- T cells was increased in SSc patients compared to controls (Mann-Whitney test p=.003).
Figure 1. Altered cytometric phenotype of circulating PD_1hi CXCR5- cells in SSc patients. (A) Heatmap of row-normalized expression of cytometry markers on indicated subsets. * indicates markers (HLA-DR, CD38) that are significantly upregulated on PD_1hiCXCR5- cells in SSc compared to controls (Bonferroni adjusted p < 0.05). (B) Biaxial gating of ICOS and HLA-DR expression on PD_1hi CXCR5- memory CD4 T cells. Frequency of PD_1hi CXCR5- HLA-DR+ ICOS- T cells was increased in SSc patients compared to controls (Mann-Whitney test p=.003).
 Figure 2. Association of CD4 T cell subset with ILD (A) Frequency of CD4+ T cells with PD_1hi CXCR5- HLA-DR+ ICOS- phenotype in SSc patients with ILD compared to controls and SSc patients without ILD (* p=0.017, ** p=0.001). (B) Correlation of PD_1hi CXCR5- HLA-DR+ ICOS- CD4+ T cells with FVCpp, DLCOpp and FEV1pp (pp=percent predicted). Spearman correlation statistics shown.
Figure 2. Association of CD4 T cell subset with ILD (A) Frequency of CD4+ T cells with PD_1hi CXCR5- HLA-DR+ ICOS- phenotype in SSc patients with ILD compared to controls and SSc patients without ILD (* p=0.017, ** p=0.001). (B) Correlation of PD_1hi CXCR5- HLA-DR+ ICOS- CD4+ T cells with FVCpp, DLCOpp and FEV1pp (pp=percent predicted). Spearman correlation statistics shown.
To cite this abstract in AMA style:
Elahee M, Mueller A, Wang R, Cao Y, Fava A, Dellaripa P, Boin F, Rao D. Expanded PD-1hi CXCR5- HLA-DR+ T Cells Is Associated with Interstitial Lung Disease in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/expanded-pd-1hi-cxcr5-hla-dr-t-cells-is-associated-with-interstitial-lung-disease-in-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/expanded-pd-1hi-cxcr5-hla-dr-t-cells-is-associated-with-interstitial-lung-disease-in-systemic-sclerosis/
