Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatoid arthritis (RA) is a chronic inflammatory condition characterized by joint inflammation and systemic involvement. In this preliminary study, we explore the potential link between two readily available hematological markers, the neutrophil-to-lymphocyte ratio (NLR) and red cell distribution width (RDW), in patients diagnosed with rheumatoid arthritis as providers of valuable insights of systemic inflammation.
To analyze the utility of the red cell distribution width (RDW) and neutrophil-to-lymphocyte ratio (NLR) as markers of disease activity in patients with rheumatoid arthritis (RA).
Methods: A longitudinal and retrospective study was conducted using data from the Cordobesian Rheumatoid Arthritis Registry (CRheAR) cohort. Clinical and biochemical data were collected at baseline and 6 months. Patients were divided into three groups based on treatment received: cDMARDs, anti-TNFα and anti-IL-6. Univariate analysis was performed to assess differences in clinical characteristics among the three groups. Receiver operating characteristic (ROC) curves and area under the curve (AUC) were used to evaluate the performance of RDW and NLR in assessing disease activity and identifying disease flare (according to the standardized definition of DAS28) using the change (Δ) in these variables between visits. Additionally, ROC curves were conducted with traditional indices (SDAI, CDAI, CRP, ESR) for comparison. Concordance between measures was assessed using the intraclass correlation coefficient (ICC).
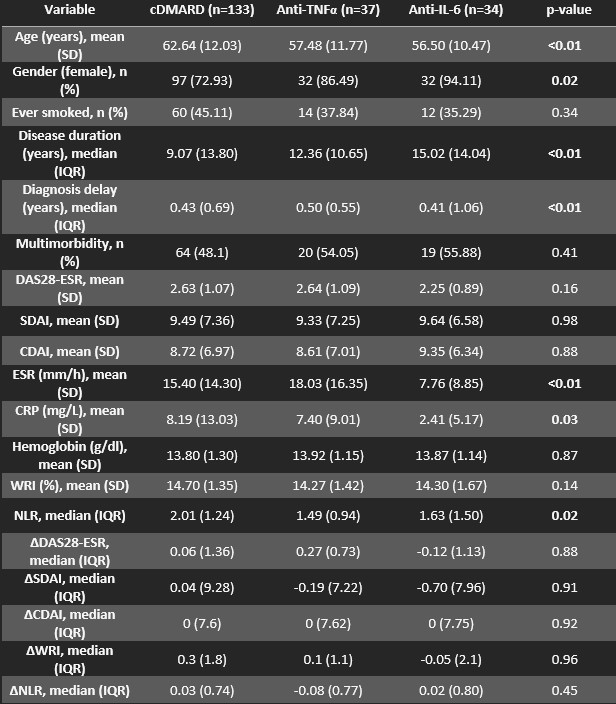
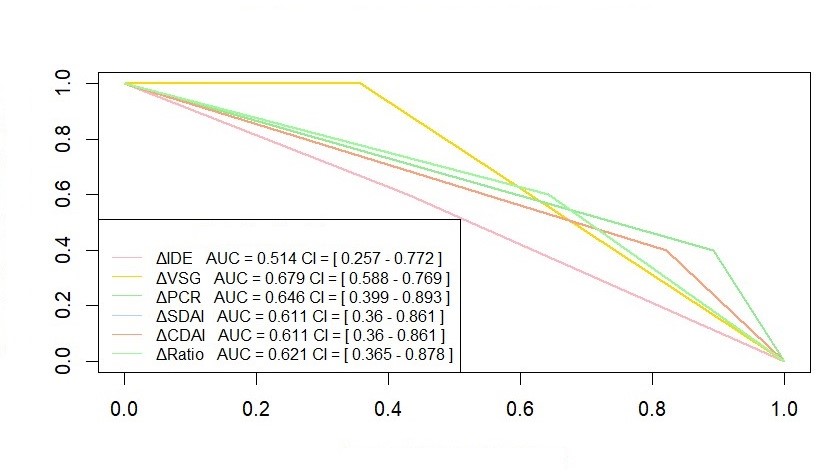
Results: A total of 204 patients were included, including 133 cDMARDs, 37 anti-TNFα, and 34 anti-IL-6. Univariate analysis is presented in Table 1. Differences were observed in disease duration (p < 0.01), with a lower median disease duration in the cDMARD group. No significant differences were observed in disease activity. In ROC curves, the neutrophil/lymphocyte ratio showed a higher AUC in the anti-IL-6 group compared to cDMARD and anti-TNFα groups (0.762; 0.511; 0.526), surpassing CRP (0.683; 0.719; 0.548) and ESR (0.566; 0.564; 0.543) in the mentioned group. However, RDW results had poorer performance (0.528; 0.642; 0.507), with a higher AUC in the cDMARD group. Regarding the identification of a “flare,” ROC curves were generated with Δneutrophil/lymphocyte ratio values in the anti-TNFα and anti-IL-6 groups (Figure 1), with slightly higher performance in the latter (0.583; 0.621), similar to CRP (0.5; 0.646) and ESR (0.583; 0.679). We also assessed the concordance of the neutrophil/lymphocyte ratio with DAS28-ESR at baseline using ICC (0.165; -0.173; 0.465 in cDMARD, anti-TNF, and anti-IL-6, respectively) and at 6 months (0.238; 0.101; 0.412), with higher concordance in the anti-IL-6 group. RDW concordance at baseline (0.101; 0.084; -0.046) and at 6 months (0.097; 0.318; -0.221) showed poor results in all groups.
Conclusion: In conclusion, the NLR demonstrates acceptable performance for identifying disease activity and flare in RA patients, especially in those treated with anti-IL-6 inhibitors, while RDW did not show additional advantages. However, further studies are needed to better understand the utility of this marker in clinical practice and its validation in other cohorts.
To cite this abstract in AMA style:
Dans Caballero S, Rojas Giménez M, López Medina C, Cid Chaves A, Rico-Muñoz M, parra Moreno m, Escudero-Contreras A. Evaluation of Width Range Index (WRI) and Neutrophil-to-Lymphocyte Ratio (NLR) in Assessing Disease Activity in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/evaluation-of-width-range-index-wri-and-neutrophil-to-lymphocyte-ratio-nlr-in-assessing-disease-activity-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluation-of-width-range-index-wri-and-neutrophil-to-lymphocyte-ratio-nlr-in-assessing-disease-activity-in-patients-with-rheumatoid-arthritis/