Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Medical evidence suggests decreased ovarian reserve in women with rheumatic disease; however, studies in adolescents are lacking. Anti-Mullerian hormone (AMH) levels in serum are shown to be a reliable marker of ovarian reserve. This study investigated the effect of pediatric rheumatic diseases, specifically adolescents meeting classification criteria for systemic lupus erythematosus (SLE), ANCA-vasculitis (AAV), Takayasu arteritis (TA), juvenile dermatomyositis (JDM), and mixed connective tissue disease (MCTD) on ovarian reserve as reflected by AMH levels.
Methods: AMH levels were collected and analyzed by quantitative ELISA from SLE, JDM, MCTD, AAV, and TA post-menarchal adolescents aged 11-20y and from menstrual age-matched, healthy controls. Demographic, menstrual, and rheumatic disease-specific characteristics were also collected. SLE disease activity, measured by SLE Disease Activity Index (SLEDAI), was evaluated in SLE and MCTD adolescents at time of enrollment. These characteristics were compared between the groups using two-sample tests and Fisher’s exact tests as appropriate. Univariate linear regression models were used to test the association of specific rheumatic disease characteristics and disease activity on AMH levels in the diseased group.
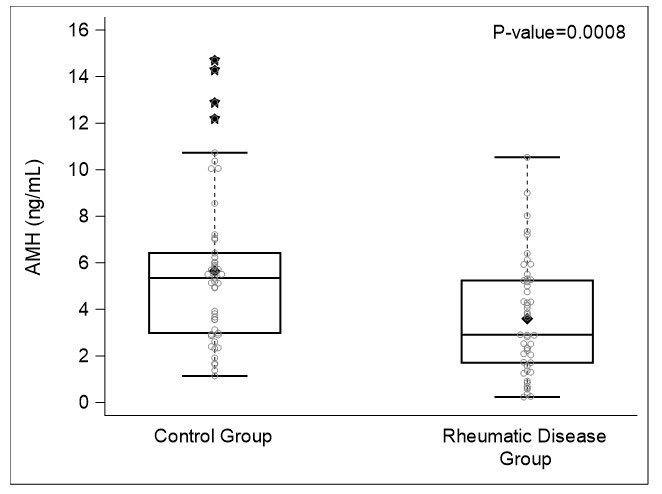
Results: Median age of adolescents with rheumatic disease was 15.8 ± 2.5 years. Median age of healthy controls was 15.1 ± 2.5 years. Age of onset of menarche corrected for race and menstrual characteristics were not significantly different from healthy controls (Table 1). Adolescents with rheumatic disease had significantly reduced AMH levels compared to healthy controls (3.6 ± 2.4 ng/mL vs. 5.6 ± 3.3 ng/mL, p=0.0008) (Figure 1). Among adolescents with SLE and MCTD, increased SLEDAI was associated with reduced AMH levels (p=0.02). AMH levels among adolescents with SLE and adolescents with other rheumatic disease were not significantly different. Prednisone exposure and evidence of cardiac involvement was associated with reduced AMH levels, whereas renal involvement, antiphospholipid antibody positivity and cyclophosphamide exposure were not significantly associated with reduced AMH levels in the diseased group (Table 2).
Conclusion: Serum AMH levels were significantly reduced in adolescents with rheumatic disease compared to menstrual-age matched, healthy controls. In adolescents with SLE and MCTD, higher disease activity was associated with reduced AMH levels. These findings suggest rheumatic disease and disease activity may affect ovarian reserve. Pediatric rheumatologists should be aware of this finding when considering their patients’ reproductive health. This pilot study indicates further studies are needed to assess the effect of pediatric rheumatologic disease on ovarian reserve.
To cite this abstract in AMA style:
Theisen A, Lane K, Skiles J, Saraf A, Tarvin S, Hannon T, Shew M, Oliver M. Evaluation of Ovarian Reserve Using Anti-Mullerian Hormone Levels in Adolescents with Systemic Rheumatic Disease Compared to Healthy Controls [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/evaluation-of-ovarian-reserve-using-anti-mullerian-hormone-levels-in-adolescents-with-systemic-rheumatic-disease-compared-to-healthy-controls/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluation-of-ovarian-reserve-using-anti-mullerian-hormone-levels-in-adolescents-with-systemic-rheumatic-disease-compared-to-healthy-controls/