Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Healthcare utilization is increasing among patients with rheumatic diseases. While several studies have assessed healthcare utilization in rheumatoid arthritis (RA) patients, few studies have assessed utilization among psoriatic arthritis (PsA) and systemic lupus erythematosus (SLE) patients. The objective of this study was to examine healthcare utilization trends among patients with RA, PsA, or SLE.
Methods: This was a cohort study of fully insured commercial or Medicare members of a large national health plan between 1/1/2018 and 1/1/2023. Members ≥ 18 years old were included if they had at least 2 visits for RA (ICD-10 code: M05 or M06), PsA (L40.5), or SLE (M32) during the study period. Members were excluded if they did not maintain continuous eligibility for 6 months before or after entrance into the study, had multiple conditions of interest, or had missing socioeconomic status (SES) data. Healthcare utilization metrics were examined as use of telemedicine, emergency room (ER), or inpatient services and were identified by place of service codes on medical claims. ER and inpatient claims were aggregated by day and are presented by days utilizing the service. Utilization rates were calculated based on total person years observed in each cohort and the sum of telemedicine claims. ER days and inpatient days are presented as claims or days per 100 person years observed. Rate differences and rate ratios were calculated with 95% confidence intervals (CI) with direct bivariable cohort comparisons. Continuous variables were assessed with analysis of variance or Kruskal-Wallis tests; categorical variables were assessed with the Chi2 test. P-values < 0.05 are significant, except for cohort comparisons of rate ratios, where the Bonferroni correction was applied and p< 0.005 is considered significant.
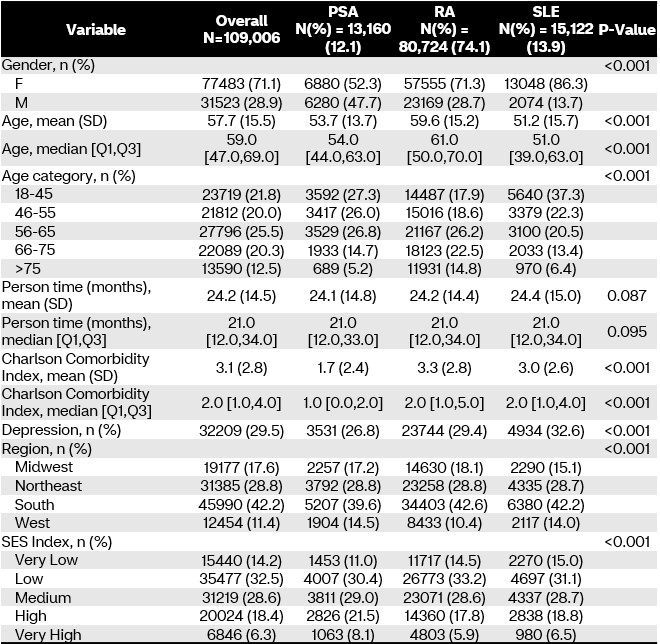
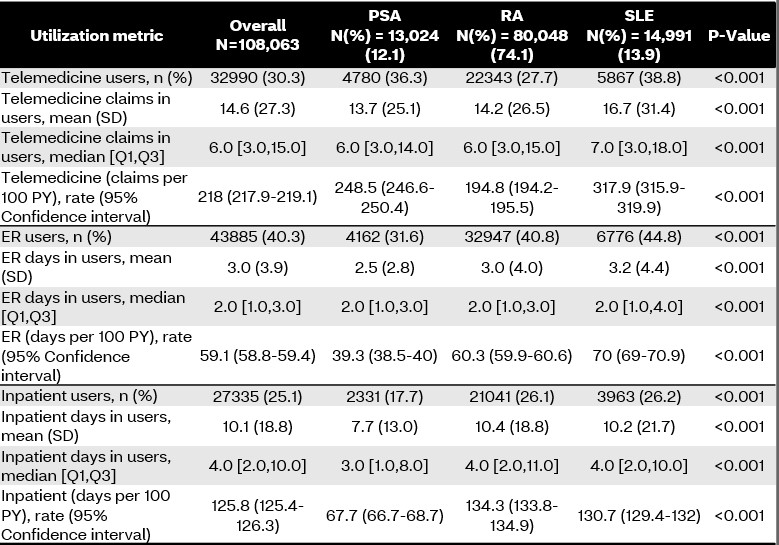
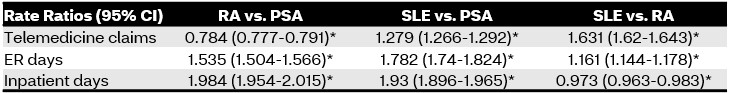
Results: Of the 109,006 members included in this study, 80,724 (74.1%) had RA, 15,122 (13.9%) had SLE, and 13,160 (12.1%) had PsA. Table 1 demonstrates significant differences in baseline demographics between disease states, with RA members being older (mean age (standard deviation (SD)): 59.6 (15.2) vs. 53.7 (13.7) and 51.2 (15.7) years in PsA and SLE members, respectively; p< 0.001) and having more comorbidities at baseline (mean Charlson Comorbidity Index (SD): 3.3 (2.8) vs. 1.7 (2.4) and 3 (2.6) in PsA and SLE members, respectively; p< 0.001). Tables 2 and 3 demonstrate the differences in healthcare utilization between disease states. In general, SLE members utilized all healthcare services more than PsA and RA members, except for inpatient services compared to RA members (rate ratio (95% CI): 0.973 (0.963-0.983); p< 0.005). Members with RA utilized ER and inpatient services significantly more than PsA members but utilized telemedicine services less (p< 0.005).
Conclusion: Members with SLE utilize significantly more healthcare services compared to RA and PsA members. In this current study it is not clear what other factors are influencing these utilization patterns. Further studies of healthcare utilization are needed in these patients.
To cite this abstract in AMA style:
Park J, Rutter W, Avalos-Reyes E, Liu C, Cavers W, Verbrugge D, Johnson K. Evaluation of Healthcare Utilization in Members with Rheumatoid Arthritis, Psoriatic Arthritis, and Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/evaluation-of-healthcare-utilization-in-members-with-rheumatoid-arthritis-psoriatic-arthritis-and-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluation-of-healthcare-utilization-in-members-with-rheumatoid-arthritis-psoriatic-arthritis-and-systemic-lupus-erythematosus/