Session Information
Date: Sunday, November 12, 2023
Title: (0609–0672) Systemic Sclerosis & Related Disorders – Clinical Poster I: Research
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The gastrointestinal (GI) tract is the second most commonly impacted organ in systemic sclerosis (SSc). However, the pathogenesis and clinical expression of GI involvement in SSc are heterogeneous. Although it is well-established that a subset of patients with SSc have co-existing dysautonomia, the type(s) of GI dysmotility seen among these patients, and the clinical and serologic features that distinguish such patients from the rest of the SSc population are unknown. Therefore, we sought to determine whether patients with SSc have a high burden of autonomic symptoms, a distinct clinical and serologic phenotype, and specific GI transit abnormalities.
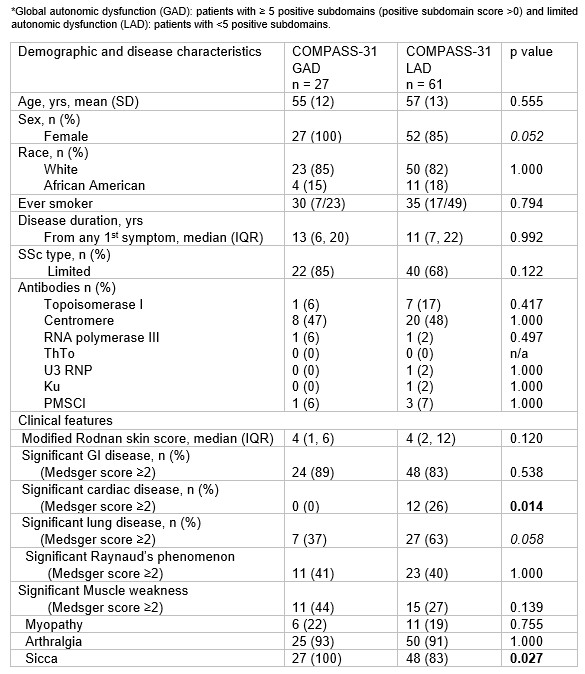
Methods: Patients were part of a prospectively enrolled cohort of SSc patients with GI disease who were evaluated at the Johns Hopkins Scleroderma Center, and demographic and clinical data for all study participants were obtained every 6 months at routine clinic visits. Autonomic symptoms were identified using the maximum obtained values of the validated Composite Autonomic Symptom Score (COMPASS)-31 questionnaire. GI transit was measured by Whole-gut transit (WGT) scintigraphy, which captures the percent emptying of the esophagus, stomach, small bowel, and colon at defined time points. The presence and severity of organ involvement were assessed using the maximum Medsger severity scores. We then sought to define the clinical and demographic features associated with significant dysautonomia in SSc. Clinical and demographic variables were compared between patients with global autonomic dysfunction [(GAD); ≥5 positive COMPASS-31 subdomains] and those with limited autonomic dysfunction [(LAD); < 5 positive subdomains] as previously defined. Differences in GI transit in across different regions of the gut were also compared between the GAD and LAD groups.
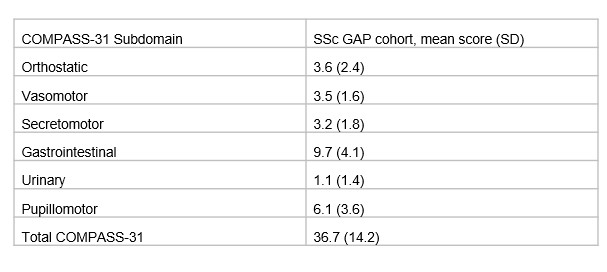
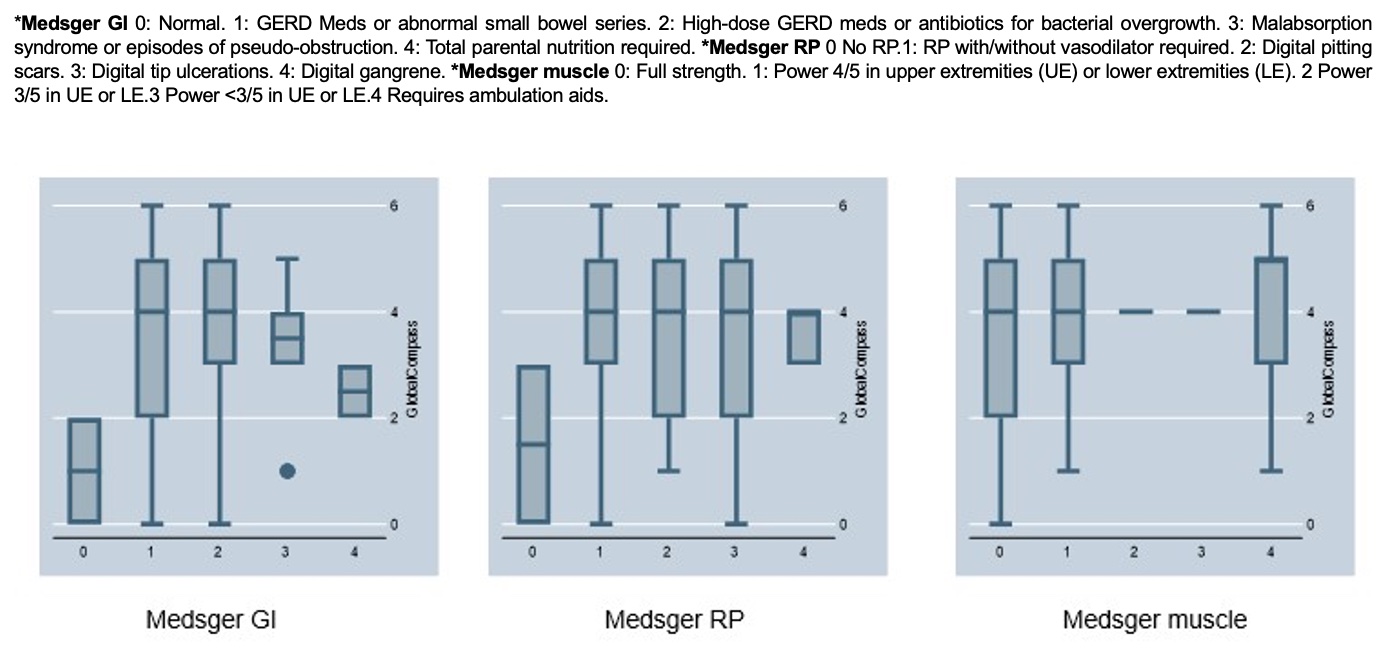
Results: The study included 99 patients with SSc and GI involvement. The mean age was 58 years (IQR 49-67), 90% were female, 74% had limited cutaneous disease, and 49% had anticentromere proteins antibodies. 83% had significant GI disease (Medsger score ≥2), and 88% had Sicca syndrome. The mean COMPASS-31 score across the cohort was 36.7 ± 14.2 (SD), which was higher overall than COMPASS-31 scores in another SSc cohort and healthy control cohorts in the published literature. We found that 31% of patients had GAD, and 69% had LAD. Patients with GAD were significantly more likely to have Sicca symptoms (100% vs. 83%; p=0.027) and less likely to have severe heart disease (0% vs. 23%; p=0.014). Patients with more severe upper GI involvement (Medsger scores 1 or 2) had higher autonomic symptom scores. All patients with Raynaud´s phenomenon (RP) and patients with severe myopathy were more likely to have higher autonomic symptoms. Patients with GAD had a higher percentage of gastric emptying of solids at 4 hours than LAD patients (97% vs 94%, respectively, p =0.023).
Conclusion: Global dysautonomia is common among patients with SSc and GI dysmotility and associated with a distinct clinical features. Identifying these clinical characteristics may help support patient risk stratification and aid in choosing the right patient population who may benefit from the evolving array of autonomic nervous system modulating therapies.
To cite this abstract in AMA style:
Alvarez Hernandez M, Adler B, Perin J, Hughes M, McMahan Z. Evaluating the Associations Between Autonomic Dysfunction, Clinical Phenotype and Gastrointestinal Transit in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/evaluating-the-associations-between-autonomic-dysfunction-clinical-phenotype-and-gastrointestinal-transit-in-patients-with-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluating-the-associations-between-autonomic-dysfunction-clinical-phenotype-and-gastrointestinal-transit-in-patients-with-systemic-sclerosis/