Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Giant-Cell Arteritis (GCA) is the most common systemic vasculitis among North Americans, historically described in Caucasian populations, with limited clinical data in other ethnic backgrounds. Despite ongoing research in the field of Rheumatology many disparities remain. Our objective was to compare the demographic, clinical characteristics, comorbid conditions, and side effects to treatment in GCA patients with different ethnic backgrounds specifically Hispanics and Caucasians.
Methods: A single center retrospective chart analysis was performed on 400 patients with associated ICD10 code diagnosis of GCA seen at Loma Linda University Health from 2013 to 2020. 53 patients with a diagnosis of GCA, based on a positive temporal artery biopsy or meeting the ACR 1990 GCA classification criteria confirmed by an expert Rheumatologist were identified. We used Pearson’s chi-square to test for independence between demographic and clinical categorical variables and ethnicity. We used independent samples t-test to test for mean differences in the continuous clinical variables between Caucasians and Hispanics and set alpha equal to 0.05 for statistical significance.
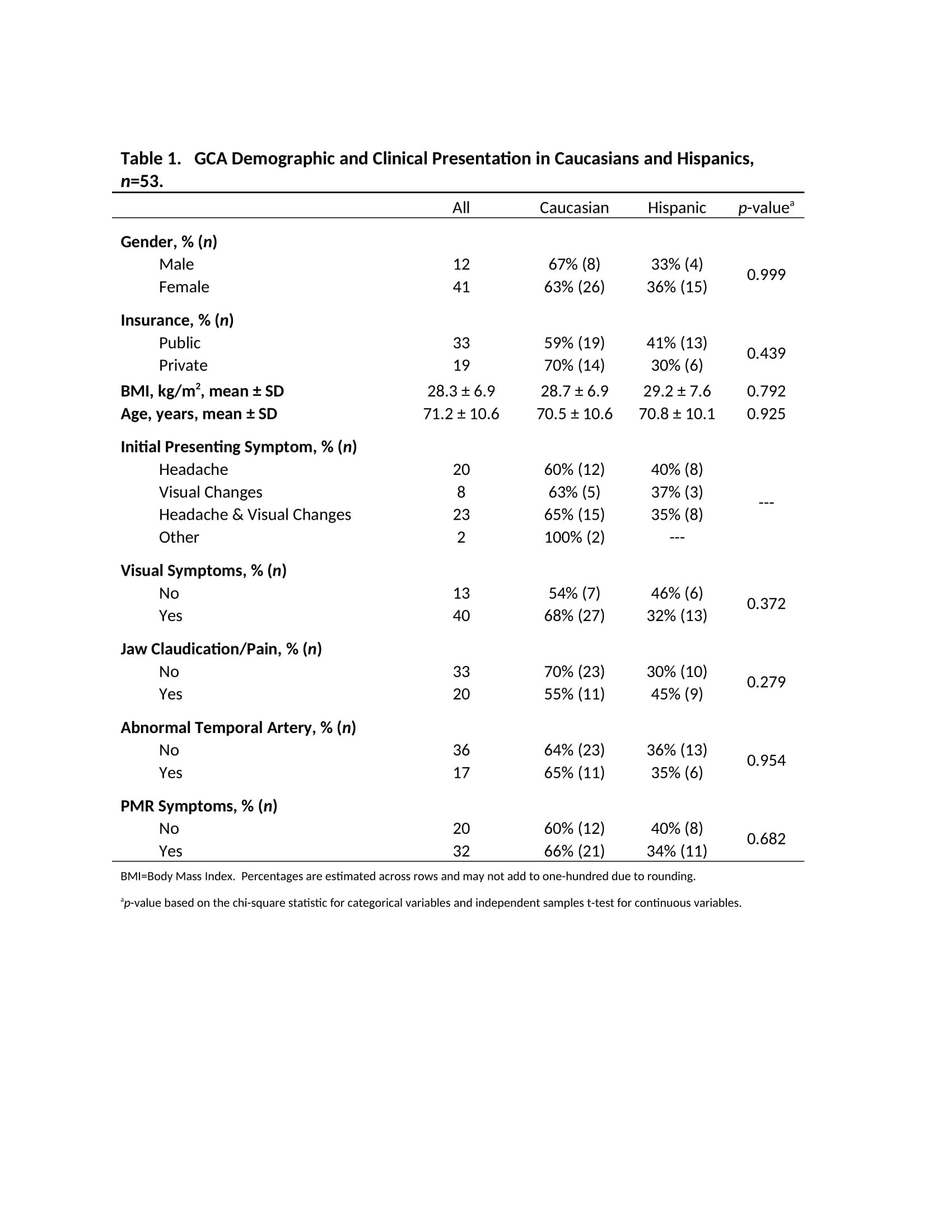
Results: We did not detect any proportional differences in average age, BMI, or gender between Caucasians and Hispanics in our cohort. A higher proportion of Caucasians had private insurance compared to Hispanics (70% vs 30%). Clinically, we found that a higher proportion of Caucasian patients reported headaches, visual symptoms, Polymyalgia Rheumatica, and had clinically documented abnormal temporal artery on physical exam at time of diagnosis when compared to Hispanics (Table 1).
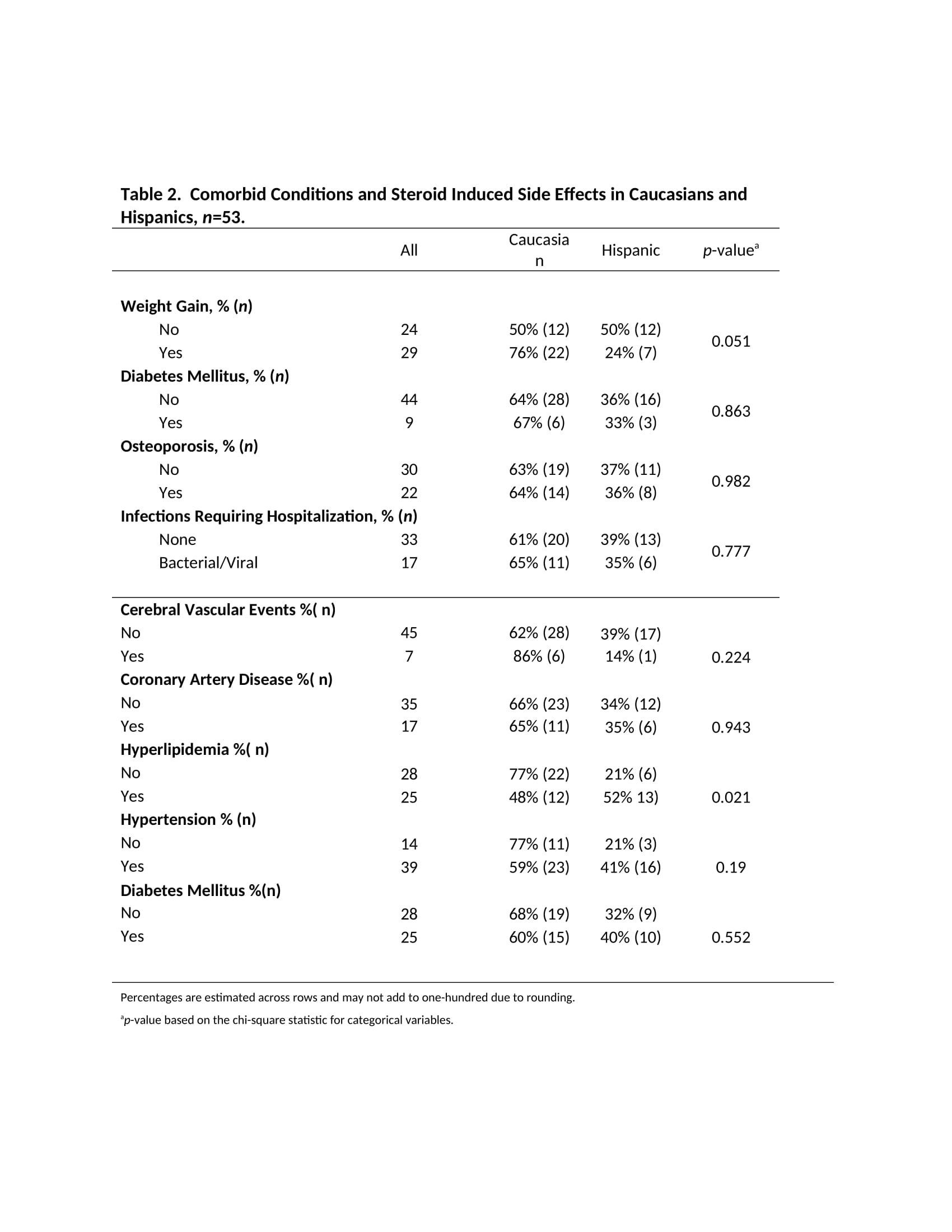
We also examined associated risk factors/comorbidities and observed that Hispanics were proportionally more likely to have a diagnosis of Hyperlipidemia (HLD) compared to Caucasians and that this difference was statistically significant (p=0.021). Caucasian patients experienced a higher proportion of steroid side effects, overall, most notably weight gain (p=0.051) while on treatment compared to the Hispanic group (Table 2).
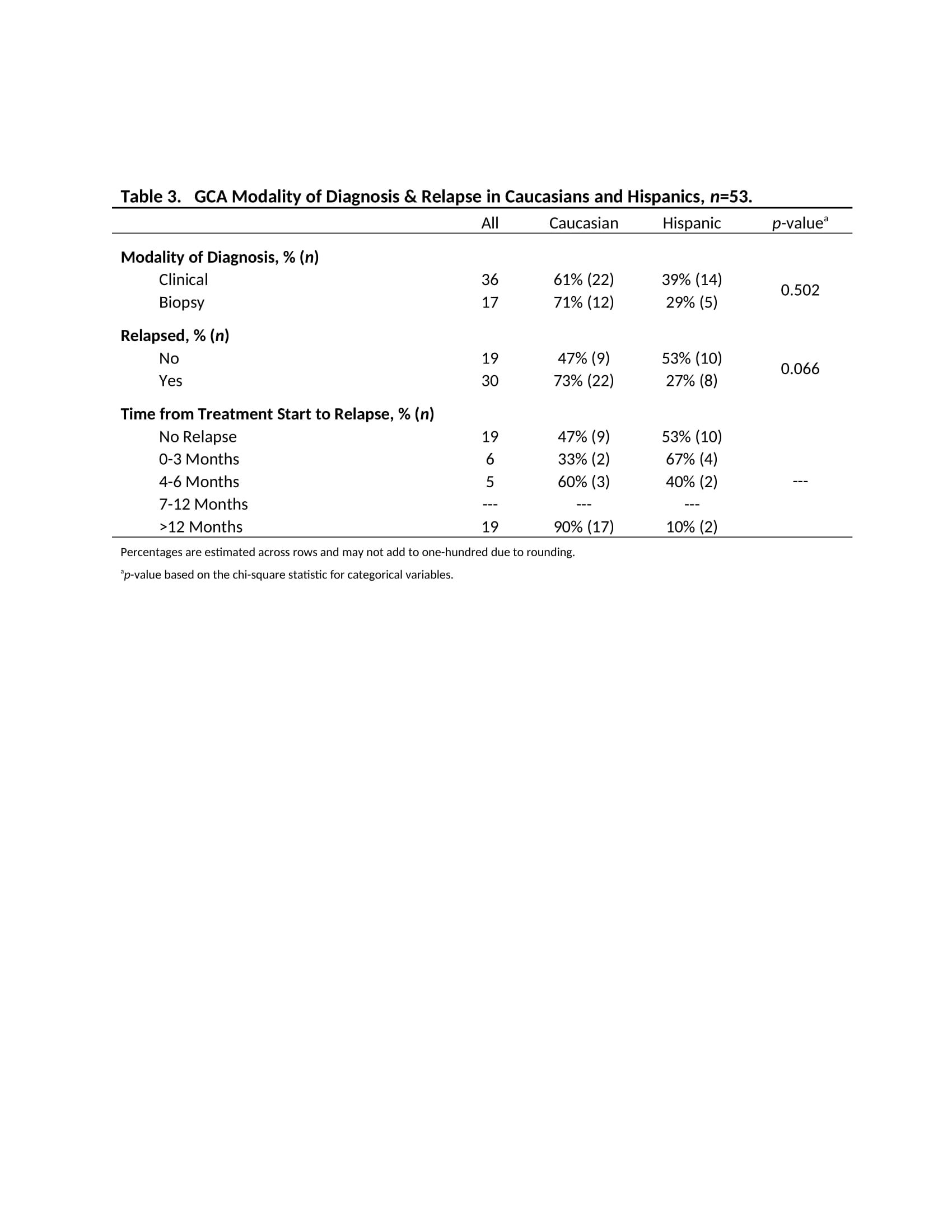
Interestingly our Caucasian cohort was more frequently diagnosed via abnormal biopsy (71% vs 29%) than the Hispanic group. We also investigated relapse data and noted Caucasians were more likely to relapse compared to Hispanics (p=0.066) and the relapse was occurring mostly after twelve months of diagnosis and treatment initiation (Table 3).
Conclusion: We observed some differences in Caucasians and Hispanics, specifically among their comorbidities, long term steroid side effects, and potential to relapse. We found that some conditions such as HLD are statistically more prevalent in our Hispanic population, while relapse and steroid side effects were more common in the Caucasian group. We also found some variations in the initial clinical manifestations in these two groups.
Further large-scale research across multiple centers with diverse populations could produce valuable insight into whether there is meaningful clinical variations or disease phenotypes based on ethnicity that can potentially affect therapeutic decisions and disease prognosis.
To cite this abstract in AMA style:
D'Anna K, Hojjati M. Ethnic Disparities in Giant-Cell Arteritis: A Clinical Comparison Among Caucasian and Hispanic Patients in the Inland Empire of Southern California [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/ethnic-disparities-in-giant-cell-arteritis-a-clinical-comparison-among-caucasian-and-hispanic-patients-in-the-inland-empire-of-southern-california/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ethnic-disparities-in-giant-cell-arteritis-a-clinical-comparison-among-caucasian-and-hispanic-patients-in-the-inland-empire-of-southern-california/