Session Information
Date: Tuesday, November 12, 2019
Title: RA – Diagnosis, Manifestations, & Outcomes Poster III: Comorbidities
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Interstitial lung disease (ILD) is the most common lung manifestation of RA and the 2nd leading cause of death in RA patients.1,2 The purpose of this literature review was to characterize the epidemiology, risk/prognostic factors, and treatment landscape of rheumatoid arthritis-associated interstitial lung disease (RA-ILD).
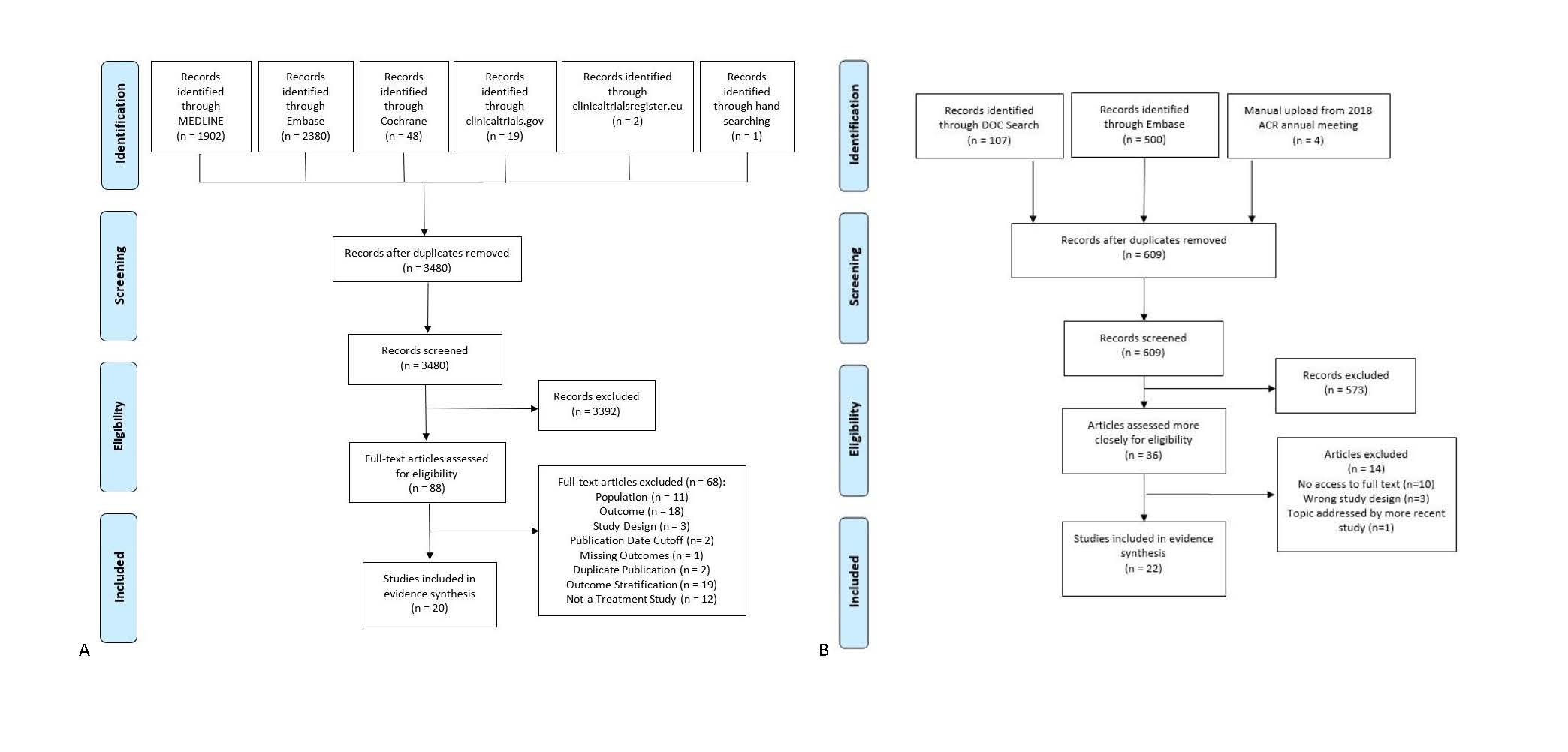
Methods: A systematic literature review was conducted by searching MEDLINE, Embase, and Cochrane CENTRAL (inception-Dec 26, 2018) supplemented by conference proceedings from ACR and EULAR, and US and European clinical trial registries (2016 to 2018). Randomized controlled trials (RCTs), non-randomized clinical trials, and observational studies that investigated therapies for adults with RA-ILD and reported efficacy and safety outcomes were included. This was supplemented by a comprehensive search using Doctor Evidence LLC’s proprietary search platform (DOC Search) containing MEDLINE, clinicaltrials.gov, WHO-ICTRP, EPAR, Daily Med, and RSS feeds, targeting the most relevant literature on the epidemiology and risk/prognostic factors associated with RA-ILD.
Results: The results of search and screening yielded 42 publications eligible for evidence synthesis; 22 studies reporting on the epidemiology and risk/prognostic factors and 20 studies (1 non-randomized clinical trial and 19 observational studies) on treatments for RA-ILD (Figure 1).
Unadjusted incidence of ILD in RA patients ranged from 1.3/1,000 person-years for interstitial pneumonia-type ILD to 5.0/1,000 person-years for “probable or definite ILD.” RA-ILD prevalence ranged widely from 1.8% to 67%. This variation is more likely attributable to the difference in sample sizes, definitions of ILD, and how ILD was diagnosed across the eligible studies. Comorbidities among patients with RA-ILD included ischemic heart disease (13%), congestive heart failure (8.5%), and diabetes (9.9%). Advanced age was the strongest predictor of developing ILD with pre-existing RA and poorer prognosis once RA-ILD was present. Male gender, RA disease duration, and anti-CCP/CCP2 positivity were also reported as important potential risk factors for ILD. Of the 6 studies that included RA drug treatments in their multivariate models assessing risk factors for ILD among RA patients, only one identified drug use (steroids) as an independent risk factor for developing ILD.
A variety of therapies were used across studies with some studies reporting classes of medication, while others were focused on specific combinations of individual therapies (Table 1). The included studies showed moderate to good effect for all therapies used in RA-ILD for DAS28, dyspnea, diffusing capacity for carbon monoxide, forced vital capacity (FVC), forced expiratory volume (FEV1), FEV1/FVC, and exacerbation of ILD. Few safety outcomes of interest were reported.
Conclusion: This review highlights epidemiology and potential risk factors (male gender, RA duration, and anti-CCP positivity) for ILD development in RA patients. Well-designed RCTs and meta-analyses are warranted to fully assess optimal treatment efficacy and safety of RA-ILD therapies.
To cite this abstract in AMA style:
Han X, Ferri L, Crocket G, Yoon S, Slanger T, Fazeli M. Epidemiology, Risk/Prognostic Factors, and Treatment Landscape in Rheumatoid Arthritis-Associated Interstitial Lung Disease: A Systematic Literature Review [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/epidemiology-risk-prognostic-factors-and-treatment-landscape-in-rheumatoid-arthritis-associated-interstitial-lung-disease-a-systematic-literature-review/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/epidemiology-risk-prognostic-factors-and-treatment-landscape-in-rheumatoid-arthritis-associated-interstitial-lung-disease-a-systematic-literature-review/