Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) is an autoimmune systemic disorder with high morbidity and mortality. Although CNS infections account for only 0.53–2.25% of all infections in patients with SLE, the mortality rate associated with infections of the central nervous system (CNS) such as meningitis and brain abscess (BA) has been reported to be 26.3–52.2%.However, in spite of increased understanding of SLE, many questions (such as epidemiology and risk factors of BA) remain unanswered. Up to date, no study has specifically examined the risk of BA in patients with SLE.We conducted a nationwide population-based cohort study to determine trends in the incidence, mortality and potential risk factors of brain abscess among patient with SLE in Taiwan from 2006 through 2018.
Methods: We identified systemic lupus erythematosus patients from the National Health Insurance research-oriented database, and compared the incidence rate of brain abscess with that among non-systemic lupus erythematosus controls. A Cox multivariable proportional hazards model was employed to evaluate the risk of BA the systemic lupus erythematosus cohort
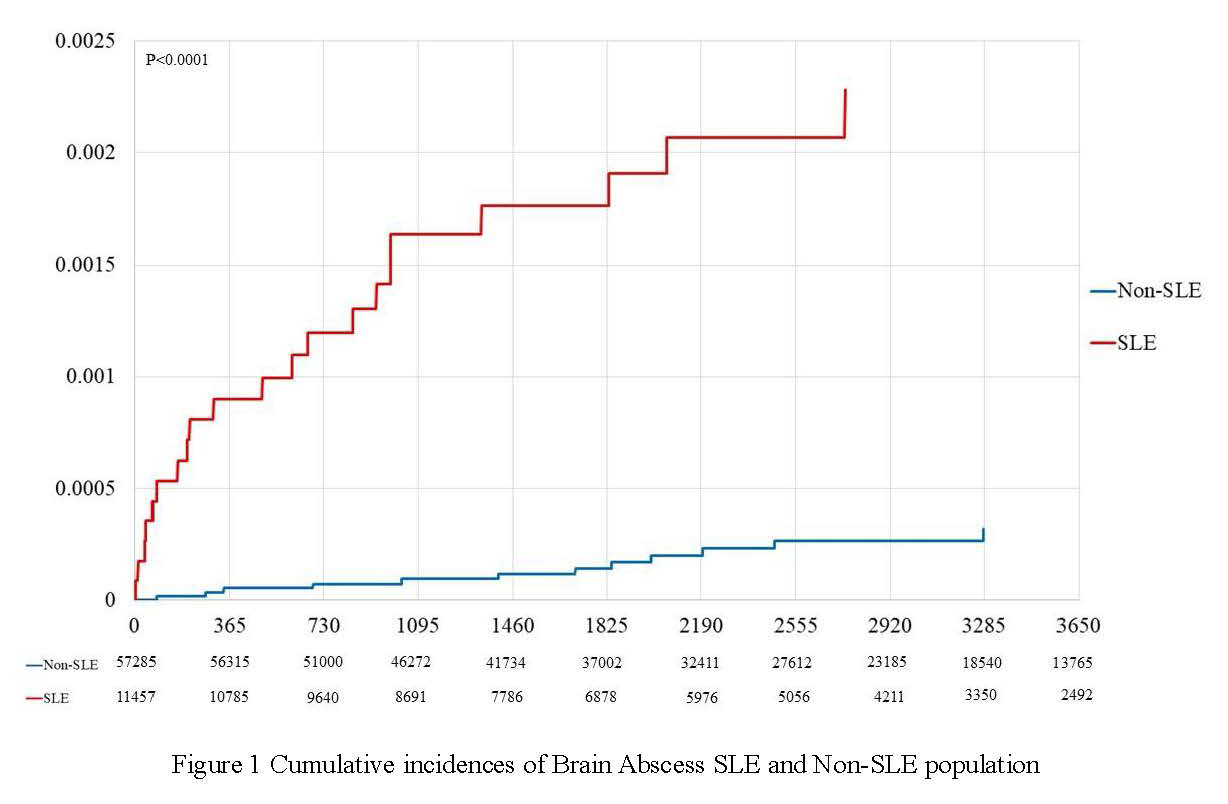
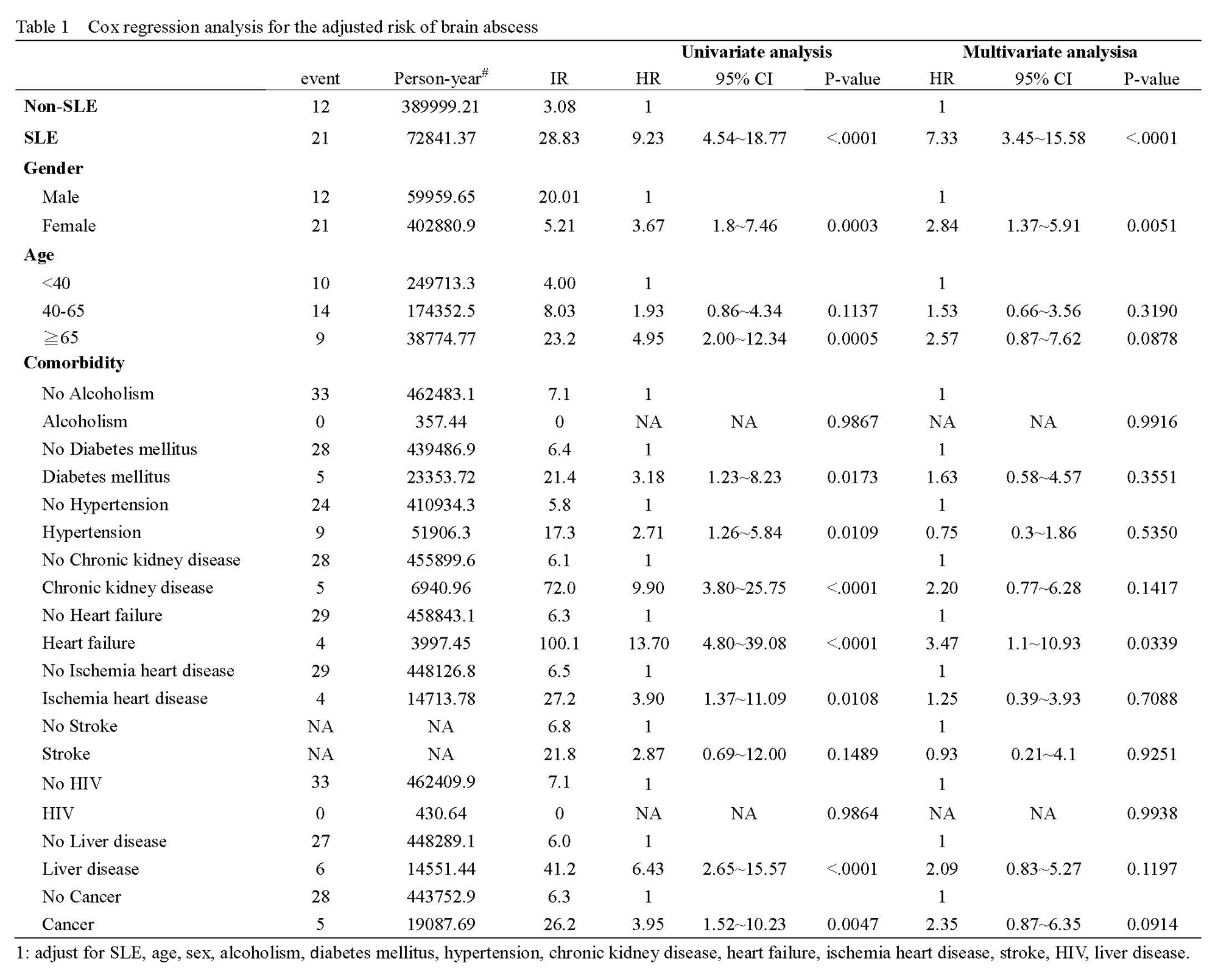
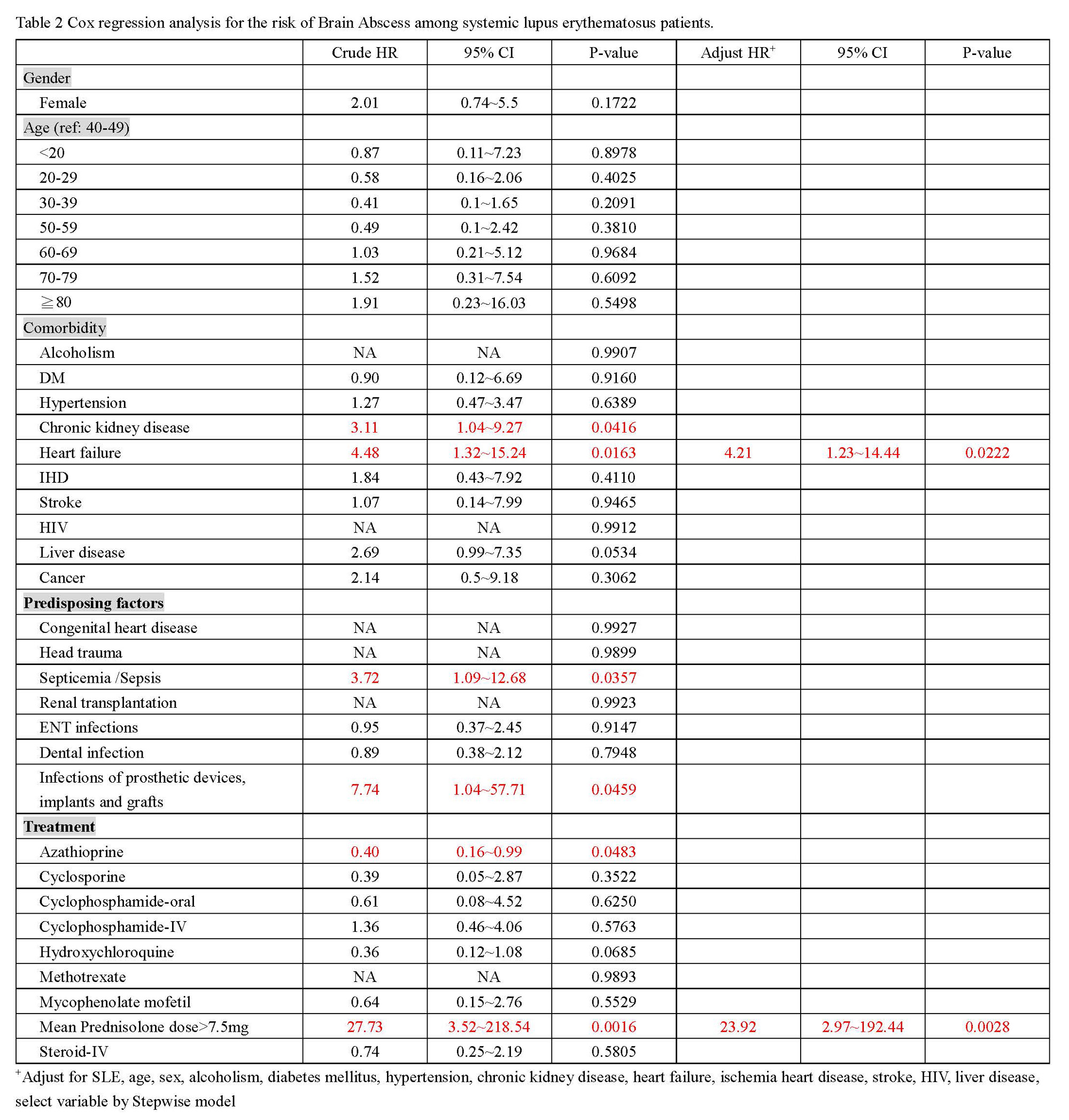
Results: We included 11,457 SLE patients and 57,285 non-SLE (mean age 42.36 yr, standard deviation 16.66yr; 85.46 % were women). After a mean follow-up of more than six years, the systemic lupus erythematosus cohort had a significantly higher incidence rate of BA (28.83 vs 3.08 per 100,000 person-years, incidence rate ratio 9.36, p<0.001, Table 1) than that of the control cohort.Kaplan–Meier analysis also revealed a significantly higher cumulative incidence of BA in the SLE patients than in the matched controls (p<0.001; Figure 1). Multivariate Cox regression analysis of the SLE and control cohorts (Table 2) revealed that SLE remained a significant risk factor even after other variables were adjusted (adjusted hazard ratio [HR] 7.33, 95% confidence interval [CI] 3.45~15.58,p<0.001). Cox multivariate proportional hazards analysis revealed heart disease (adjusted HR 4.21, [CI] 1.23~14.44), and receiving a mean prednisolone dose >7.5mg (adjusted HR 23.92, [CI] 2.97~192.44) were independent risk factors for brain abscess in systemic lupus erythematosus patients.
Conclusion: A higher risk of BA was observed in systemic lupus erythematosus patients. Risk factors for BA in the systemic lupus erythematosus cohort included heart disease, and receiving a mean prednisolone dose >7.5mg
To cite this abstract in AMA style:
Lin K, Lin T, Chang C. Epidemiology and Risk of Brain Abscess in Patients with Systemic Lupus Erythematosus in Taiwan: A Nationwide Population-based Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/epidemiology-and-risk-of-brain-abscess-in-patients-with-systemic-lupus-erythematosus-in-taiwan-a-nationwide-population-based-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/epidemiology-and-risk-of-brain-abscess-in-patients-with-systemic-lupus-erythematosus-in-taiwan-a-nationwide-population-based-study/