Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: The prevalence of Raynaud’s phenomenon (RP) in the general population is ~3-5%, of which 80–90% are primary. Autoimmune diseases are the most common causes of secondary RP, others may include vibrating tools, drugs, hematologic, vascular, or neurological diseases. A seasonal pattern with worsening RP in winter has been observed. However, the impact on RP hospitalizations in a larger sample has not been studied. The aims of this study were to study the seasonal variations in RP hospitalizations in the U.S and explore the differences in RP hospitalizations based on the presence of autoimmune rheumatic diseases (ARDs).
Methods: We used the National Inpatient Sample (NIS), the largest publicly available inpatient database in the US, to identify adults ≥18 years with a primary hospitalization diagnosis of RP from 2016 to 2019 using the ICD-10 codes I73.00 and I73.01. We used Edwards’ geometric model to analyze the seasonal variation of RP hospitalizations. Pearson’s chi-squared and t-tests were used to compare the characteristics of RP hospitalizations with and without an underlying ARD.
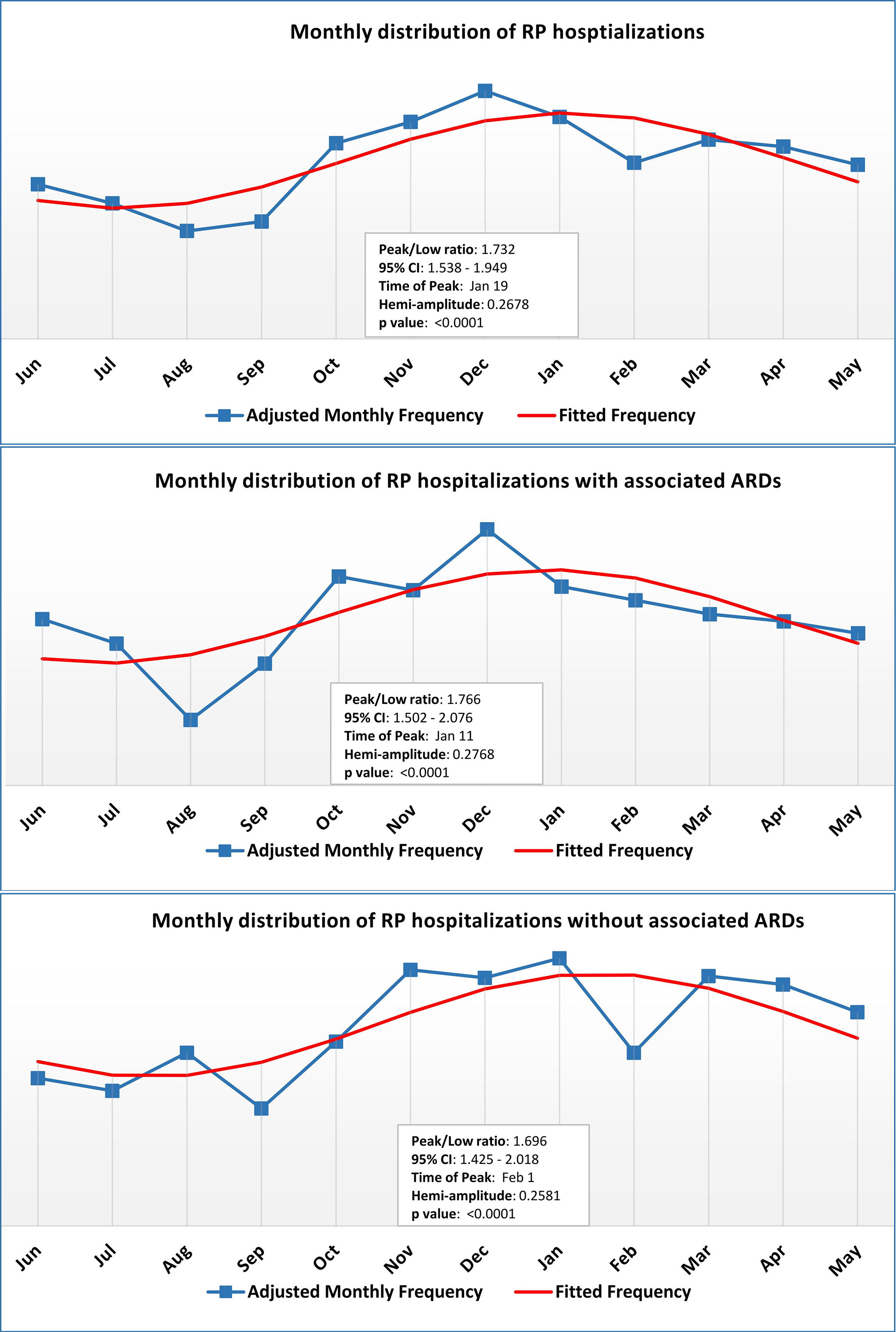
Results: We identified 2,540 hospitalizations with RP (mean age 54±0.8 years; females 77%), highest in winter (30.31%) and lowest in summer (18.50%). The fitted frequency curve showed the peak incidence to be on Jan 19 (peak/low ratio 1.73, 95% CI 1.54-1.95). Trends were similar for RP hospitalizations with or without an underlying ARD (Fig 1).
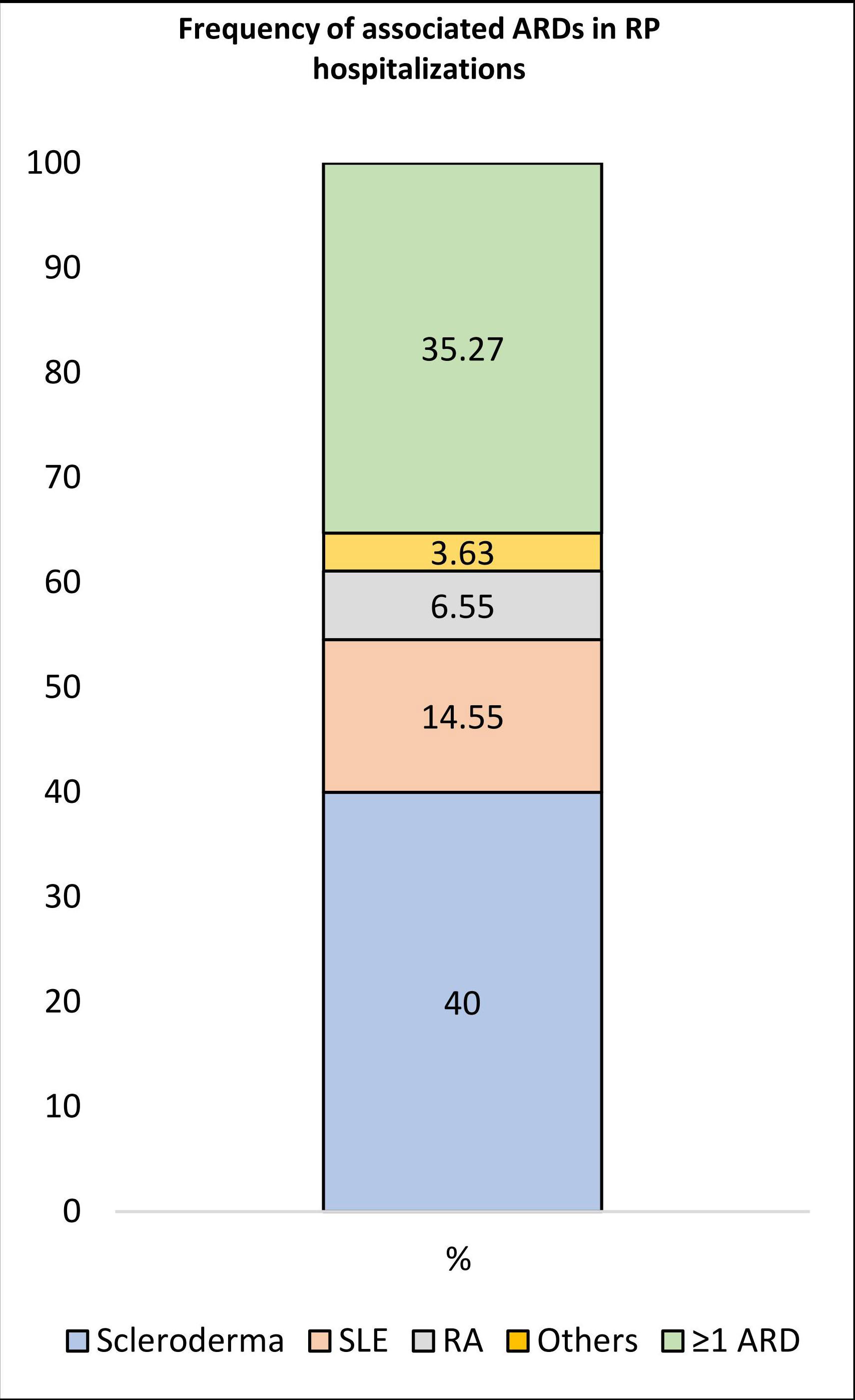
Of 2,540 hospitalized RP, 1,210 (48%) and 1,330 (52%) were RP with and without gangrene, respectively. Overall, 1,375/2,540 (54%) hospitalized RP had an associated ARD, of which 35% had ≥ 2 ARDs. The association with ARDs was higher in RP with gangrene (815, 67%) than without gangrene (560, 42%). When RP hospitalizations with a single ARD diagnosis were isolated, scleroderma (40%), SLE (14.6%), and RA (6.6%) were most common. Interestingly, while Sjogren’s was noted in ~11% with RP, 95% of those were in association with another ARD (Fig 2).
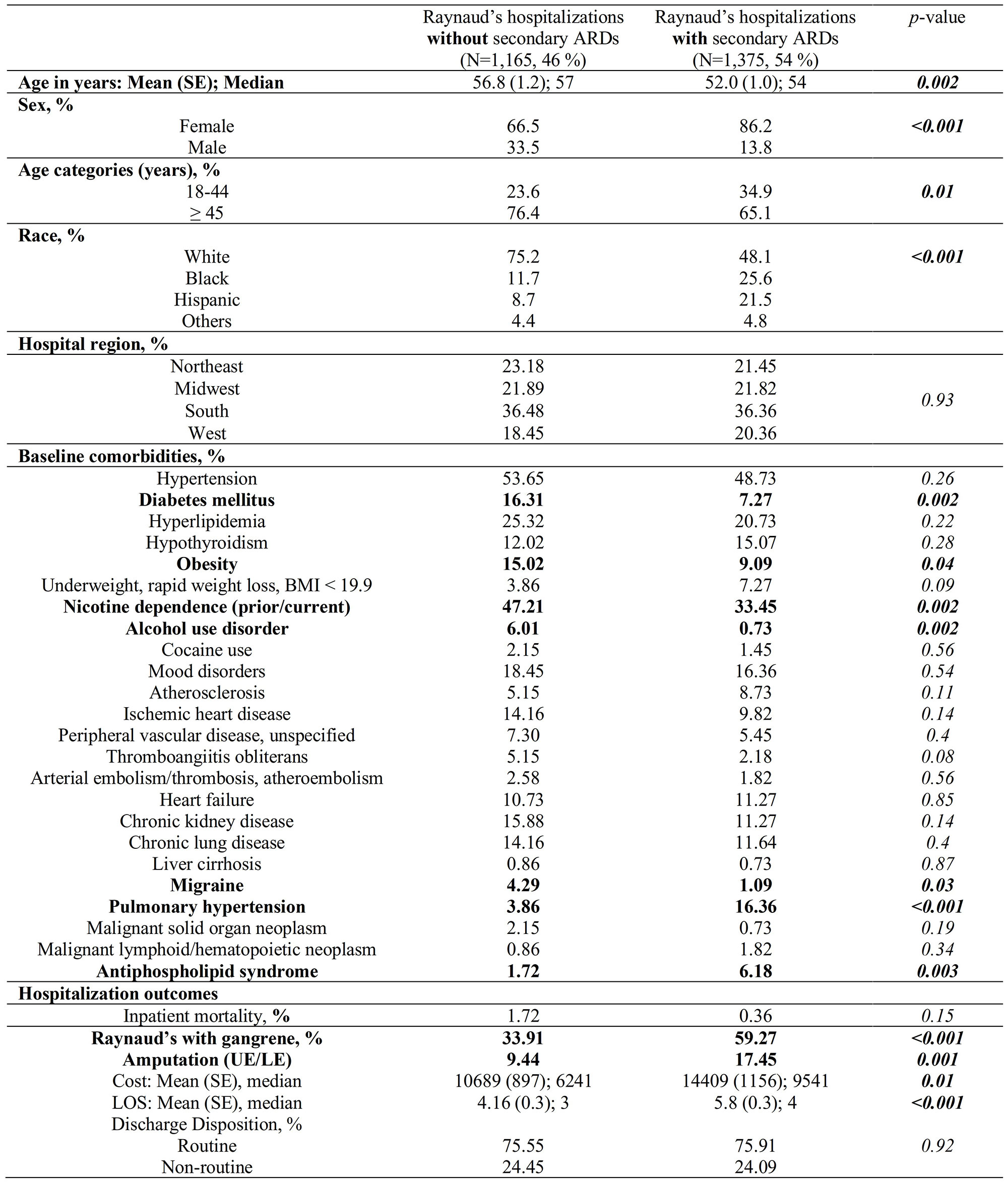
Hospitalized RP with ARDs had a significantly higher women: men ratio (6x versus 2x, p< 0.001) and Black and Hispanic patients compared to RP without ARDs (25.6 vs 11.7%, and 21.5 vs 8.7%, respectively, p< 0.001). More RPs with ARDs had a concurrent diagnosis of pulmonary hypertension (16.36% vs 3.86%, p< 0.001). On the other hand, hospitalized RP without ARDs consisted of a higher proportion (%) of patients ≥ 45 years old (76.4 vs 65.1, p 0.001) and were associated with tobacco use (47.21 vs 33.45, p 0.002), alcohol use (6.01 vs 0.73, p 0.002), obesity (15.02 vs 9.09, p 0.04), diabetes (16.31 vs 7.27, p 0.002), and migraine (4.29 vs 1.09, p 0.03). The rate of amputation was higher in RP with ARD (17.45% vs 9.44%, p 0.001) (Table 1).
Conclusion:
ARDs most associated with RP hospitalization were scleroderma and SLE. RP with ARDs comprised of higher Black and Hispanic patients, likely related to racial differences in the prevalence of underlying ARDs. RP without ARDs had a higher proportion of tobacco and alcohol use, obesity, and diabetes, suggesting their role in severe RP. As expected, the RP hospitalizations in the U.S. peaked in winter and were lowest in summer; such seasonal variation in hospitalizations might have an implication on dynamically tailoring pharmacotherapy by season.
To cite this abstract in AMA style:
Dhital R, Guma M, Lwin T, Suwal A, Pedersen B. Epidemiology and Outcomes of Raynaud’s Phenomenon Hospitalizations in the US [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/epidemiology-and-outcomes-of-raynauds-phenomenon-hospitalizations-in-the-us/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/epidemiology-and-outcomes-of-raynauds-phenomenon-hospitalizations-in-the-us/