Session Information
Date: Monday, November 14, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Patients with autoimmune rheumatic diseases presenting to the emergency department (ED) often have multi-organ pathology. SLE patients may be particularly prone to ED visits due to disease complexity, flares, medication burden and non-adherence. Only a few studies have assessed ED use in SLE. We aim to characterize the ED visits in SLE patients using the largest all-payer ED database in the US, the national emergency database sample (NEDS).
Methods: Using the 2019 NEDS database, we compared the differences in baseline demographic characteristics, clinical comorbidities, and ED outcomes in SLE adults to those without SLE. NEDS contains ~ 20% sample from 989 hospital-owned US EDs. We identified SLE using ICD-10 code M32.xx. We used multivariable logistic regression to assess factors associated with inpatient admission from the ED. We also studied the top ten primary diagnoses among SLE and age and sex-matched controls without SLE, as well as among SLE ED visits admitted versus released from the ED. We used STATA v13 for analysis.
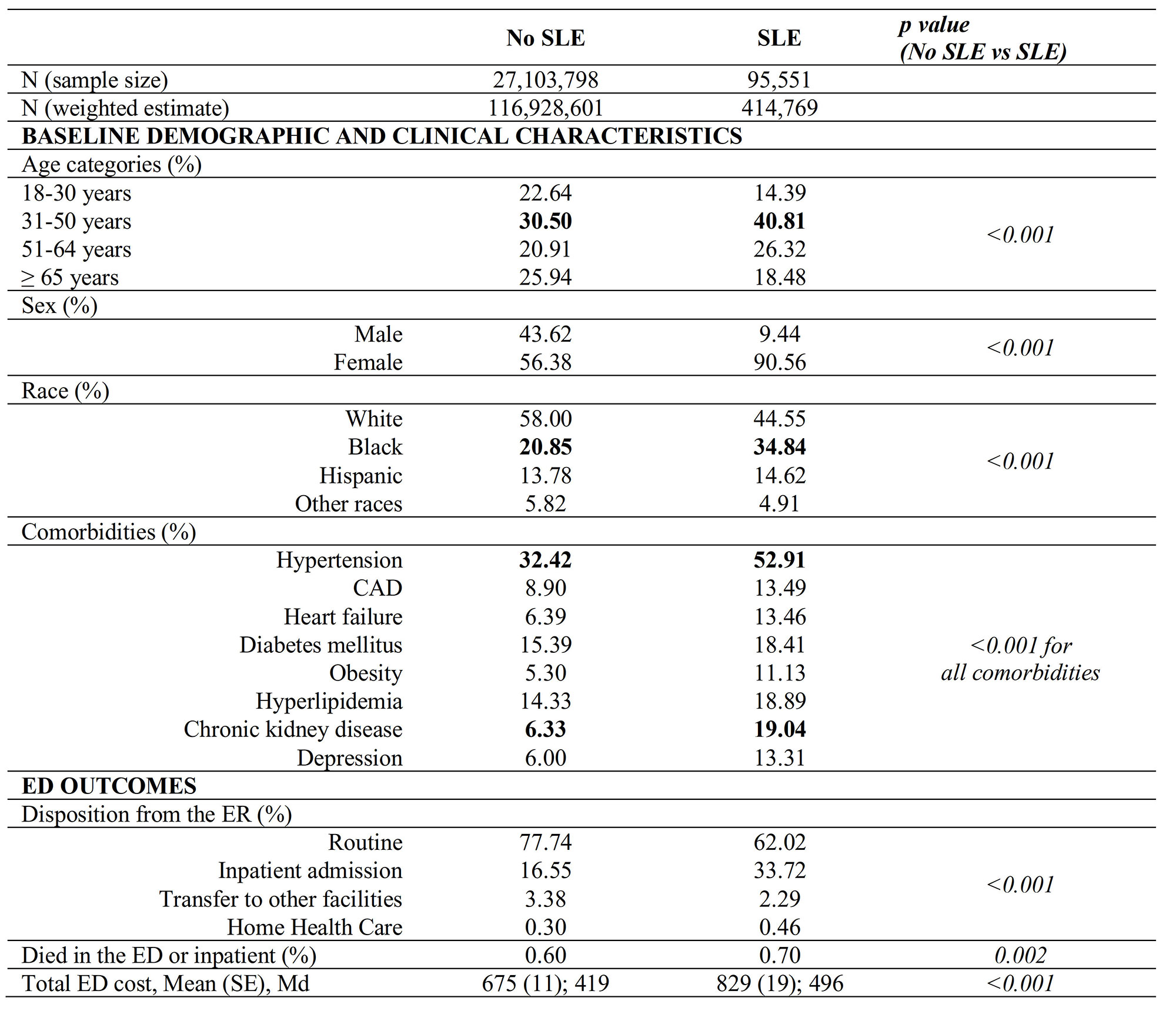
Results: Of 117,343,370 ED visits for adults ≥ 18 years in 2019, 414,769 had SLE. As expected, ED visits in SLE patients comprised of a higher proportion of women (91% vs 56%), non-Whites (55% vs 42%), and patients 31-50 years old (41% versus 31 %) than the non-SLE group, p < 0.001. All the studied comorbidities were significantly higher in SLE, the most prevalent were hypertension (53%) and chronic kidney disease (CKD, 19%) (Table 1). Men with SLE had double the prevalence of coronary artery disease (22.8% vs 12.5%), and CKD (31.2% vs 17.8%) than women, whereas obesity and depression were higher in women (11.4% vs 8.5%, and 13.6% vs 10.3%, respectively)
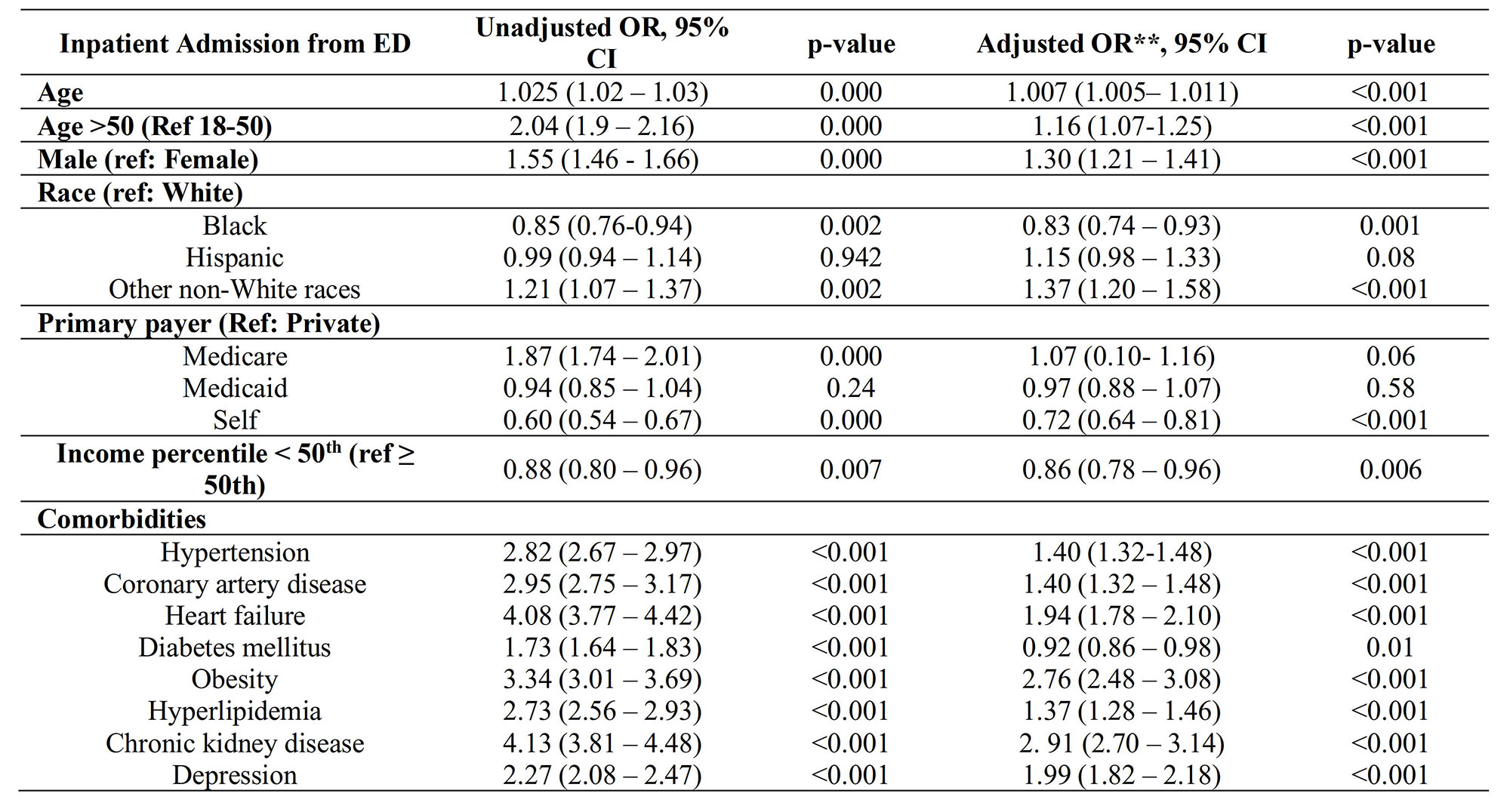
SLE ED had double the rate of inpatient admission (34 % vs 17%) and higher odds (OR, 95% CI) of admission than non-SLE (2.20, 2.03-2.37) even after adjustment for baseline characteristics and comorbidities. Age >50 years (ref: 18-50; 1.16, 1.07-1.25), and male sex (1.30, 1.21 – 1.4) were associated with higher odds of inpatient admission in SLE. The comorbidities with the highest odds of admission were CKD (2.91, 2.70-3.14) and obesity (2.76, 2.48-3.08). Black race (0.83, 0.74-0.93) and low income (0.86, 0.78-0.96) were associated with lower odds of admission, despite comprising a sizeable proportion of ED visits (Table 2).
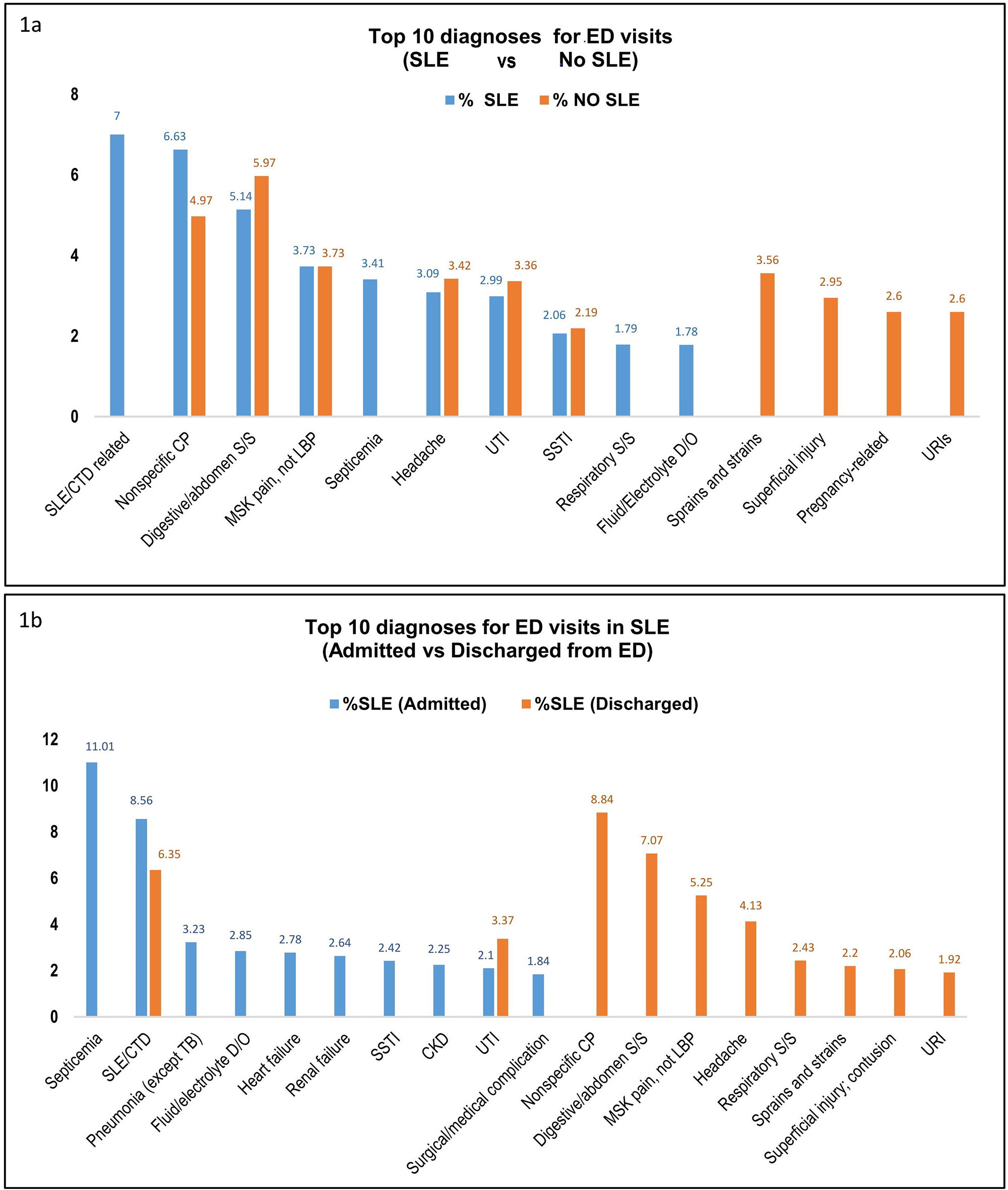
Pain-related visits were among the top causes of ED visits in both SLE and non-SLE groups. Other top diagnoses for ED visits in SLE were “SLE” and infections. The major primary diagnoses for ED visits in SLE patients who got admitted were septicemia (11.01%), SLE (8.56%), and pneumonia (2.32%) (Figure1).
Conclusion: SLE ED visits had a higher comorbidity burden than non-SLE. Male sex and most of the studied comorbidities were associated with higher rates of inpatient admission from the ED. Aggressive comorbidity management may alter higher ED and inpatient use in SLE patients. Black and low income SLE patients had higher odds for treat-and-release ED visits (as also noted in prior studies), raising a possibility that these patients may rely on ED for more routine care needs as well as socioeconomic biases on the part of healthcare providers, further research is needed to better understand these differences.
To cite this abstract in AMA style:
Dhital R, Guma M, Pedersen B, Pokharel A, Kalunian K. Epidemiology and Outcomes of Emergency Department Visits in Systemic Lupus Erythematosus: Data from National Emergency Database Sample [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/epidemiology-and-outcomes-of-emergency-department-visits-in-systemic-lupus-erythematosus-data-from-national-emergency-database-sample/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/epidemiology-and-outcomes-of-emergency-department-visits-in-systemic-lupus-erythematosus-data-from-national-emergency-database-sample/