Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Factors that identify cardiovascular disease (CVD) fully in RA are lacking. Peripheral blood mononuclear cell (PBMC) subsets in RA patients differ markedly, on average, from non-RA controls in T-cell activation/differentiation to memory effector status and in the degree monocytes exhibit an intermediate ‘inflammatory’ phenotype. We hypothesized that elevations in these subpopulations would distinguish those with subclinical atherosclerosis.
Methods: Patients with RA and no clinical CVD underwent cardiac computed tomography (CT). Coronary arterial calcium (CAC) was quantified by the Agatston method. PBMC subsets were assessed by multiparameter flow cytometry. Multivariable linear and logistic regression were used to assess the associations between PBMC subpopulations and CAC, adjusting for relevant confounders associated both with PBMC subsets of interest and CAC. The area under the receiver operator curve (AUC) was used to estimate the contribution of covariates on the prediction of any CAC.
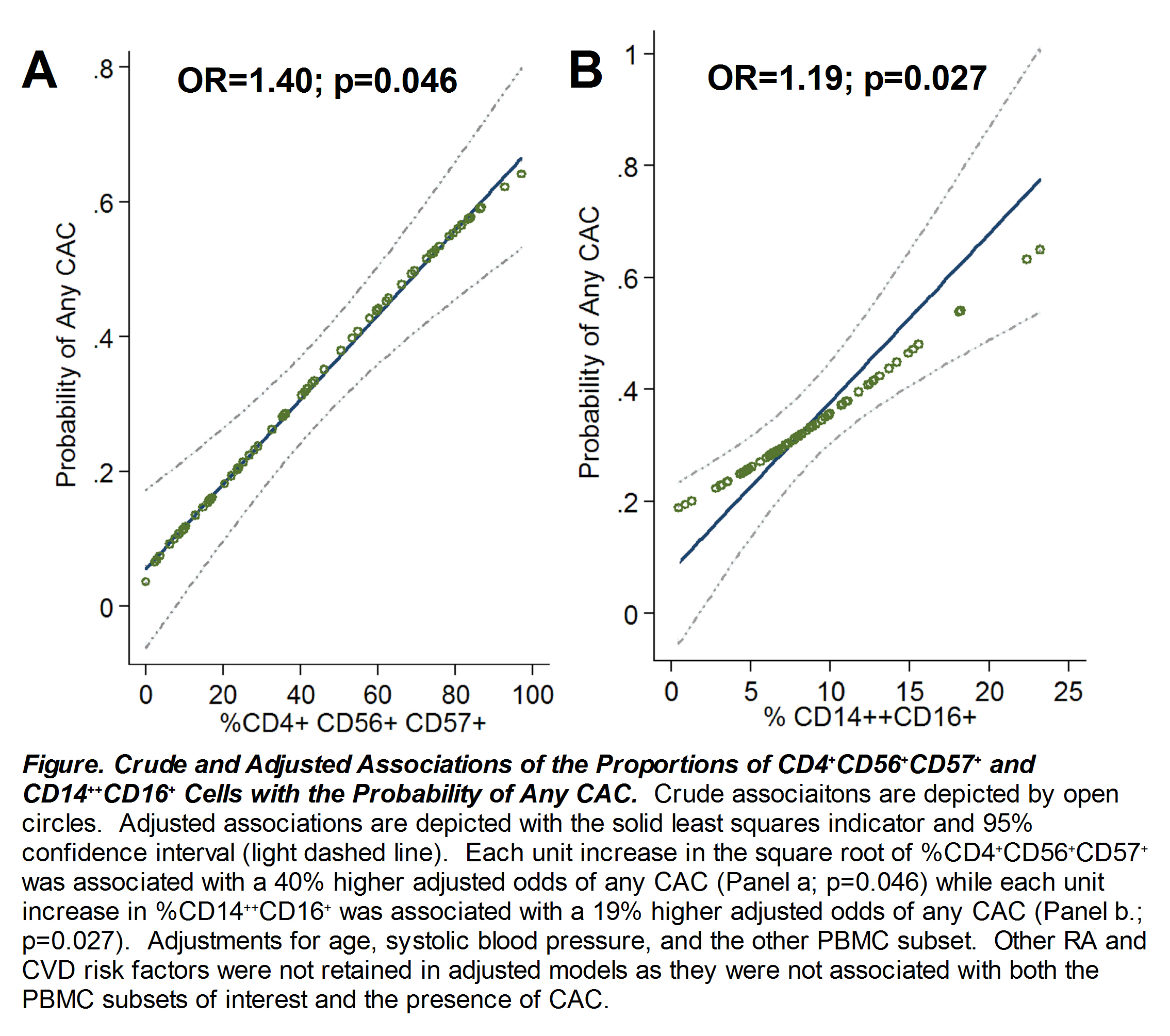
Results: 72 RA patients [mean age 54±14 years; 84% female; shared epitope positive=64%, median RA duration=6.6 years; median DAS28=3.9; current biologic use in 31%] were studied. Any CAC [CAC>0] was observed in 34%. In univariate analyses, compared with patients with no CAC, those with CAC had significantly higher percentages of circulating CD4 T cell subsets denoting activation (CD4+HLA-DR+, CD4+CD28–HLA-DR+), differentiation to memory effector (CD4+CD28–HLA-DR+, CD4+CD56+CD57+), and acquisition of NK receptors (CD4+CD56+CD57+) and similar increases of analogous CD8 T cell subsets, along with increases in the proportion of intermediate CD14++CD16+monocytes. The CD4 and CD8 subsets were highly correlated, while the CD14++CD16+monocyte subset was independent of the CD4 and CD8 subsets. In multivariable models including all non-collinear PBMC subsets of interest, only levels of CD4+CD56+CD57+ T cells and CD14hiCD16+monocytes remained significantly associated with the presence of CAC after adjusting for relevant RA and CVD risk factors (Figure). CRP, serum IL-6 and DAS28 were not associated with CAC. The AUC for any CAC for the model containing only the two PBMC subsets of interest was 0.76 (95%CI=0.64-0.87), this increased to 0.89 (95%CI 0.82-0.96) with the addition of age and systolic blood pressure to the model. Neither PBMC subset of interest was associated with the extent of CAC within those with a positive CAC score.
Conclusion: Subclinical atherosclerosis was robustly associated with levels of circulating PBMCs reflecting differentiation to memory effector status/acquisition of NK receptors and higher levels of intermediate (inflammatory) monocytes, independent of demographics, CVD risk factors, and, importantly, RA disease activity and severity. These factors may account for a portion of the unexplained contributors to enhanced atherogenesis in RA.
Disclosure:
R. Winchester,
None;
J. T. Giles,
None;
S. Nativ,
None;
H. Z. Zhang,
None;
K. Downer,
None;
J. Bathon,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/elevations-of-certain-memory-effector-t-cell-and-inflammatory-monocyte-subpopulations-in-rheumatoid-arthritis-are-associated-with-the-presence-of-subclinical-coronary-artery-atherosclerosis/