Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Individual cohort studies have found that Black and Hispanic women have worse pregnancy outcomes compared to their white counterparts. Additionally, this population of women has a higher prevalence of lupus nephritis. Therefore, this individual participant meta-analysis pooled data from multiple lupus pregnancy cohorts to assess the effect of maternal race and nephritis on pregnancy outcomes.
Methods: PubMed, Embase, and the Cochrane Database of Systematic Reviews were searched for prospective cohorts of pregnancies among women with lupus. Data from each cohort was collected and analyzed individually. Race was classified as white or non-white. Outcomes of interest included fetal loss, preterm birth (< 37 weeks gestation), preeclampsia, and high disease activity (PGA ever >1 or SLEDAI ever >4 during pregnancy). Pooled ORs were calculated in Review Manager. The analysis included one pregnancy per patient in women with a first trimester visit.
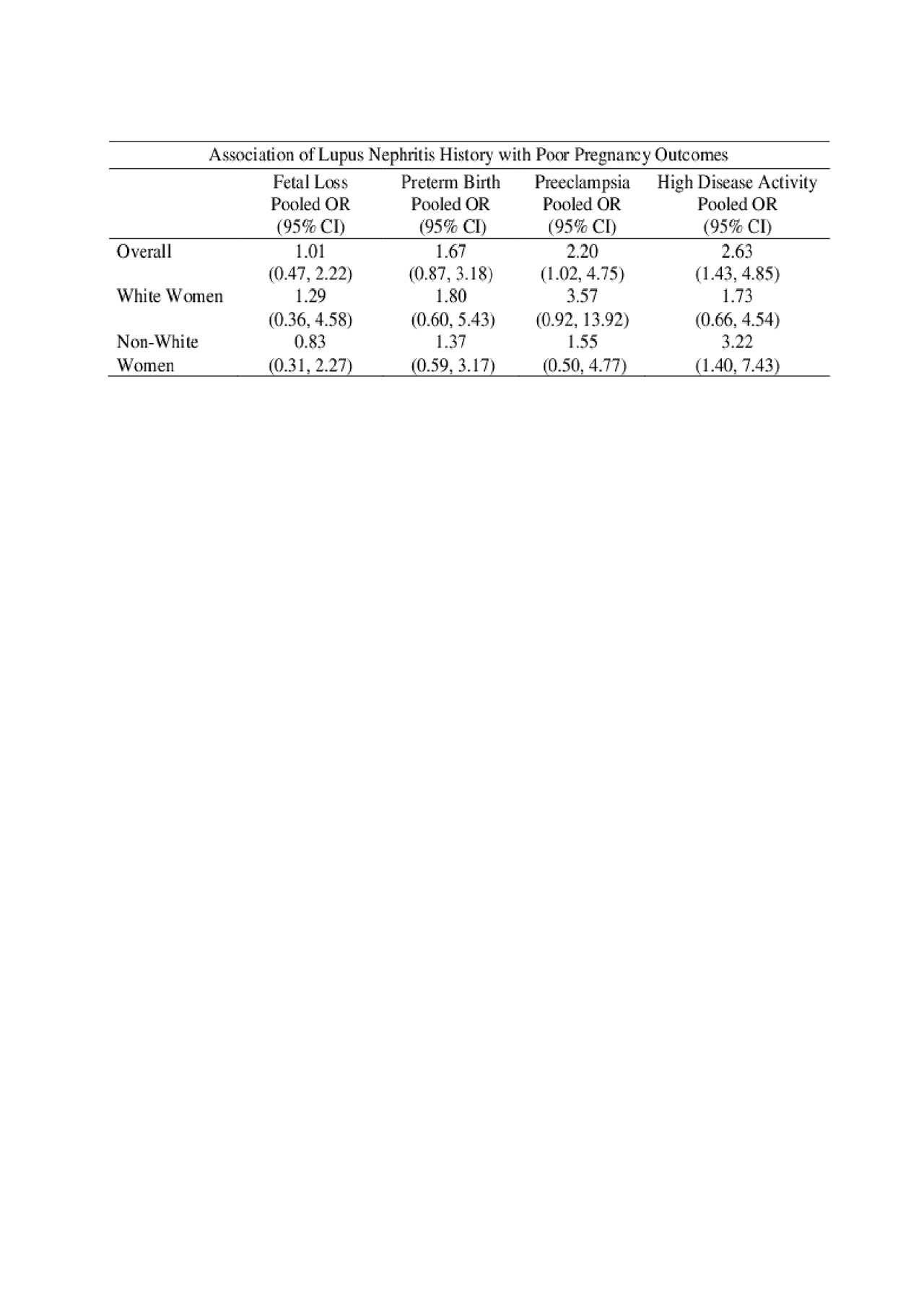
Results: The analysis included 312 pregnancies across three cohorts in the United States and Canada, of which 46% were to non-white mothers and 22% were to women with history of nephritis. Overall, there was an increased risk of fetal loss among non-white patients compared to white patients (OR: 1.96; 95% CI: 1.02,3.77). History of nephritis did not have an association with fetal loss. In patients with no nephritis history, non-white women had a higher rate of fetal loss (OR: 2.16; 95% CI: 1.03,4.52). There was no significant effect of race on preterm birth overall, nor when stratified by history of nephritis . Overall, there was no significant effect of race on preeclampsia. Among white women, a history of nephritis increased the risk of preeclampsia (OR: 3.57; 95% CI: 0.92, 13.92). Overall, non-white patients were at increased risk of high disease activity during pregnancy (OR: 1.74; 95% CI: 0.99, 3.05). Among non-white women, history of nephritis increased the risk of high disease activity during pregnancy (OR: 3.22; 95% CI: 1.40-7.43).
Conclusion: Race is not the only factor driving health disparities in pregnancy outcomes among women with lupus. Additionally, these differences are not entirely explained by the increased prevalence of nephritis in non-white women. When managing lupus in pregnancy, race and history of nephritis are important considerations. However, additional studies are needed to further elucidate why non-white women continue to have disproportionately worse outcomes.
To cite this abstract in AMA style:
Njagu R, Eudy A, Balevic S, Petri M, Gladman D, Urowitz M, Clowse M. Effect of Race and Lupus Nephritis on Pregnancy Outcomes in Systemic Lupus Erythematosus: An Individual Participant Meta-analysis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/effect-of-race-and-lupus-nephritis-on-pregnancy-outcomes-in-systemic-lupus-erythematosus-an-individual-participant-meta-analysis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effect-of-race-and-lupus-nephritis-on-pregnancy-outcomes-in-systemic-lupus-erythematosus-an-individual-participant-meta-analysis/