Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Cardiovascular (CV) risk in RA is increased due to interaction between traditional risk factors and systemic inflammation. The purpose of this analysis was to investigate the effect of biologic DMARDs on lipid levels and cardiovascular risk and evaluate whether such effect is associated with changes in CRP and disease activity measures. In addition, we evaluated whether patients with lower LDL levels experience larger increases in LDL which are tracking with disease improvement after initiation of a biologic.
Methods: Patients (pts) with at least moderate disease activity (CDAI >10) initiating a biologic DMARD enrolled in the CERTAIN comparative effectiveness study nested within CorEvitas (formerly known as Corrona) RA registry. Characteristics, including lipid values, and Reynolds Risk Score (RRS) in pts initiating a TNF-α inhibitor (TNFi) or non‐TNFi (rituximab [RTX], abatacept [ABT] or tocilizumab [TCZ]), were measured at baseline prior to biologic initiation and at 3 and 6 months later. Longitudinal mixed models examined the association of individual biologics with changes in lipid levels, and Reynolds Risk Score (RRS). Structural equation models were utilized to model mediation of CRP, CDAI or swollen joint count on lipid changes. Patients who interrupted therapy prior to follow up visits or without complete lipid data were excluded. Change in LDL at 6 months among patients with low LDL at baseline (≤90mg/dl) vs patients in groups with higher levels (90-130 and ≥130mg/dl) were compared. The association between LDL change across baseline LDL groups and disease activity improvement was evaluated.
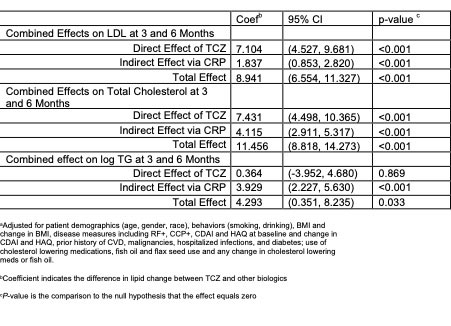
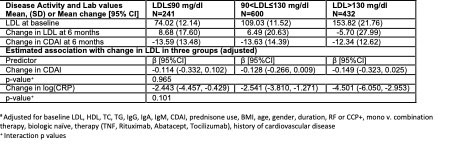
Results: 1698 initiations of a biologic were analyzed. At baseline 36.8% of pts were biologic naïve and 24.5% on anti-hyperlipidemic therapy. History of prior CVD was present in 7.9% of pts. Pts initiating TCZ had a significant increase in lipid levels but RRS at 3 and 6 months was similar across all biologics (table 1). Mediator analyses were statistically significant regarding the CRP effect (table 2). LDL changes differed depending on baseline LDL but were consistent with estimated changes due to regression to the mean. An association between LDL improvement and CRP change was similar for all baseline LDL groups (table 3).
Conclusion: The impact of lipid changes on CVD risk must be considered in the context of the burden of inflammation in pts with RA. Lipid increases may not necessarily be atherogenic and may occur in the context of the “lipid paradox”. In this analysis, moderate increases in lipid levels did not translate to an increased CVD risk as captured by RRS and were partially associated with CRP changes.
To cite this abstract in AMA style:
Pappas D, Giles J, Reed G, Kane K, Curtis J, Kremer J. Effect of Biologic Agents on Lipid Levels and Cardiovascular Risk in Rheumatoid Arthritis Patients [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/effect-of-biologic-agents-on-lipid-levels-and-cardiovascular-risk-in-rheumatoid-arthritis-patients/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effect-of-biologic-agents-on-lipid-levels-and-cardiovascular-risk-in-rheumatoid-arthritis-patients/