Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Myositis autoantibodies have diagnostic, therapeutic and prognostic implications, but their utility in clinical practice is unclear. We aimed to describe our institutionÕs ordering practices and positivity rate in an undiagnosed population of patients to improve utilization.
Methods:
We included all Duke University Health System patients who had a myositis autoantibody panel (including anti-Jo-1, PL-7, PL-12, EJ, OJ, Mi-2, SRP, PM/Scl, Ku and U2-snRNP) ordered between October 2014 and December 2015. We recorded autoantibody positivity, demographics, past medical history, family history, review of systems items (ROS) and physical examination (PE) findings. FisherÕs exact and t-tests were performed for statistical significance.
Results:
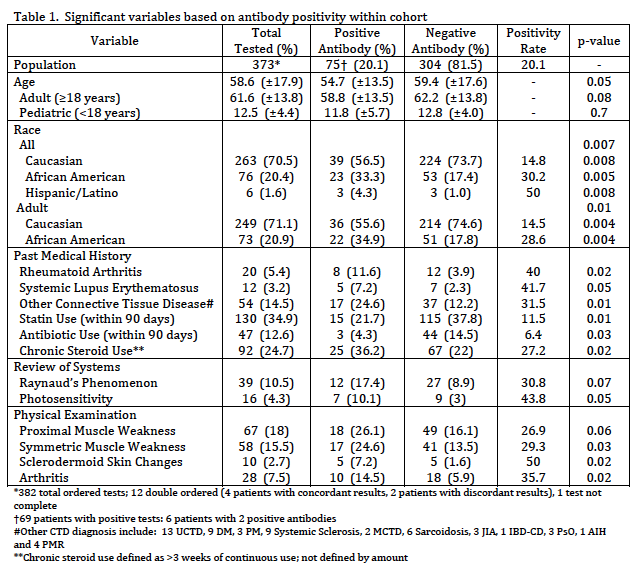
Of 373 ordered tests, there were 75 (20%) positive autoantibodies. Significant demographic factors were older age and African American race or Hispanic ethnicity (Table 1). Positivity rates among African Americans (30%) and Hispanic/Latinos (50%) were higher than in Caucasians (15%; 71% of the tested population). A recorded past medical history of RA, SLE or connective tissue disease were associated with positive autoantibodies, while use of statins, antibiotics or chronic steroids had a negative association. The only statistically significant ROS factor was photosensitivity. Important ROS elements were infrequently documented prior to testing in this cohort. Specifically, <50% of tested patients were asked about myalgias, 20% about photosensitivity, 13% about voice changes and 3% about nasal regurgitation. Of recorded PE findings symmetric muscle weakness, sclerodermoid skin changes and arthritis were significantly associated with a positive antibody test.
Conclusion:
Myositis autoantibodies were positive in more than 30% of African American and Hispanic individuals tested. History of an autoimmune disease, photosensitivity and expected IIM PE findings were associated with a positive panel. While many easily obtainable factors may be associated with positive myositis autoantibodies, these history, PE and ROS elements are incompletely recorded. In our large academic multispecialty practice, the myositis autoantibody panel appears to be largely used as a screening test. Future efforts will include cohort characterization and provider education to guide testing.
To cite this abstract in AMA style:
Weiner J, Jessee R, Eudy AM, Keenan RT, Datto M, Criscione-Schreiber L. Easily Obtainable Myositis Autoantibody Panel Predictive Factors [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/easily-obtainable-myositis-autoantibody-panel-predictive-factors/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/easily-obtainable-myositis-autoantibody-panel-predictive-factors/