Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with axial spondyloarthritis (axSpA) bear a substantial burden of chronic opioid use despite the availability of effective treatments like tumor necrosis factor inhibitors (TNFi). It remains uncertain whether initiating TNFi treatment earlier can reduce the risk of long-term opioid use. We assessed whether early TNF inhibitor use is linked to a decreased risk of subsequent chronic opioid use among individuals newly diagnosed axSpA.
Methods: We conducted a propensity score (PS)-matched cohort study of incident axSpA using the Merative™ MarketScan® Database. We included adults aged 18-65 with ≥1 inpatient or ≥2 outpatient axSpA ICD-9 or 10 diagnosis codes separated by ≥7 days, with continuous enrollment for ≥18 months from 2006-2021. The diagnosis date was the date of the first axSpA ICD code. We excluded patients with rheumatoid arthritis codes or TNFi prescriptions in the 12 months preceding the axSpA diagnosis.
The exposure of interest was early TNFi initiation, defined as any TNFi prescription within 6 months following the diagnosis date. The primary outcome was chronic opioid use, defined as >90 days of consecutive prescriptions (allowing gaps ≤30 days), assessed for all individuals starting from 6 months after the diagnosis date. Patients were followed until the outcome, end of continuous health plan enrollment, or the end of the study (12/2021).
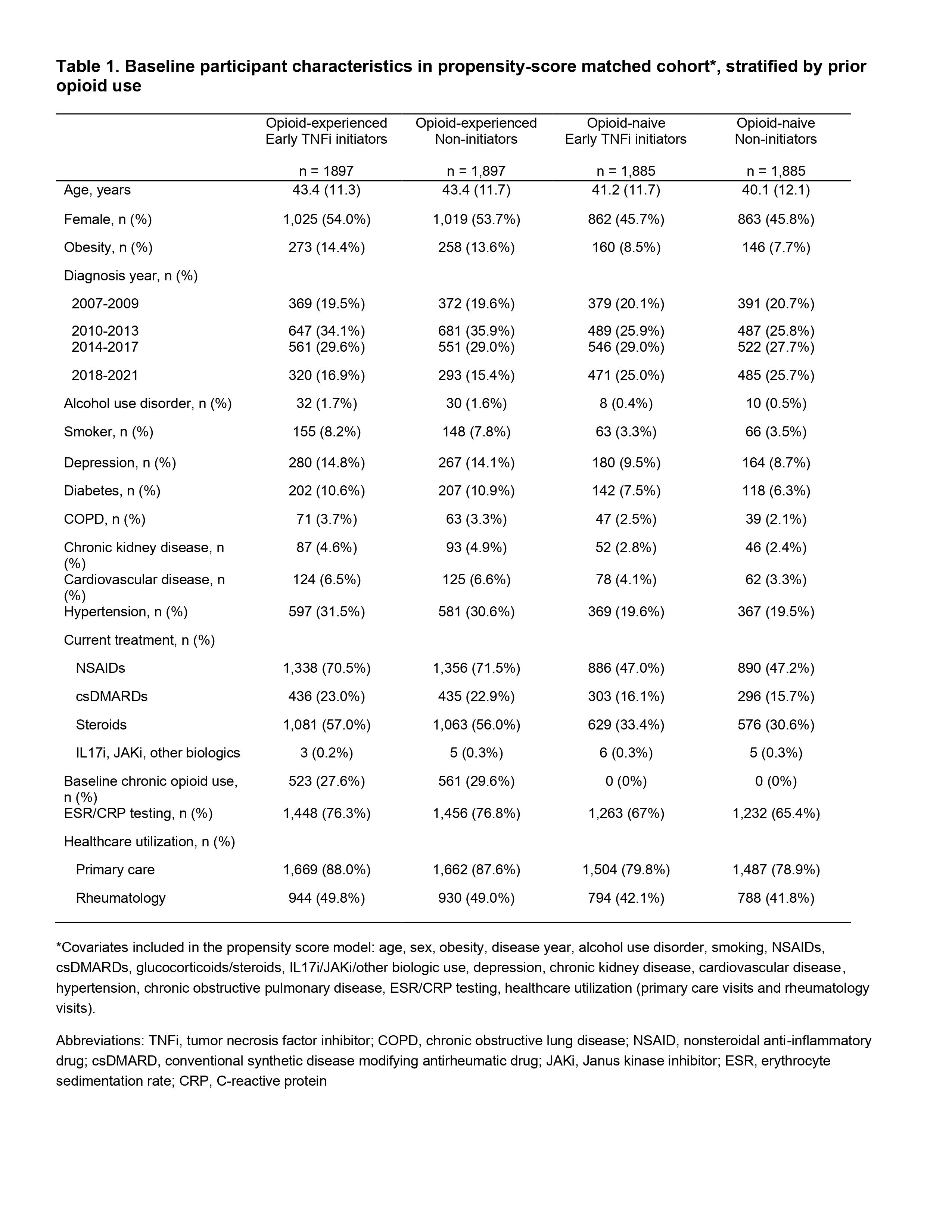
For propensity scores, we used logistic regression to estimate the probability of early TNFi initiation, accounting for covariates assessed 12 months preceding the diagnosis date (demographics, comorbidities, and surrogates for axSpA disease activity including healthcare utilization). We matched early TNFi initiators 1:1 to non-early initiators using greedy matching. To assess the relationship between early TNFi initiation and the risk of chronic opioid use we used propensity-score matched Cox regression models, stratified by prior opioid use (opioid experienced vs. naive) identified in the prior 12 months.
Results: We identified 3794 individuals with incident axSpA who were opioid-experienced (median age 43 years, 54% female), and 3770 individuals who were opioid-naive (median age 41 years, 46% female). From the opioid-experienced cohort, 1084 (29%) had chronic opioid use at baseline. Among all early TNFi initiators, 869 (23%) developed chronic opioid use, compared to 712 (19%) in non-initiators, with a mean follow-up time of 2 years.
In the opioid-experienced cohort, early TNFi initiators did not have a significantly different risk of chronic opioid use compared to non-early initiators (hazard ratio (HR) 1.01, 95% confidence interval (CI) 0.91-1.12). In the opioid-naive cohort, early TNFi initiation was associated with a higher risk of chronic opioid use compared to non-early initiation (HR 1.91, 95% CI 1.44-2.55). Results from both cohorts remained consistent with further confounder adjustment.
Conclusion: Using a large US insurance claims database, we did not see a protective association between early TNFi initiation and chronic opioid use, when accounting for prior opioid use. Interpretation of results is limited by confounding by indication.
*Covariates included in the propensity score model: age, sex, obesity, disease year, alcohol use disorder, smoking, NSAIDs, csDMARDs, glucocorticoids/steroids, IL17i/JAKi/other biologic use, depression, chronic kidney disease, cardiovascular disease, hypertension, chronic obstructive pulmonary disease, ESR/CRP testing, healthcare utilization (primary care visits and rheumatology visits).
Abbreviations: TNFi, tumor necrosis factor inhibitor; COPD, chronic obstructive lung disease; NSAID, nonsteroidal anti-inflammatory drug; csDMARD, conventional synthetic disease modifying antirheumatic drug; JAKi, Janus kinase inhibitor; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein
To cite this abstract in AMA style:
Petrow E, Meade Aguilar J, Peloquin C, Jafarzadeh S, Neogi T, Dubreuil M, Liew J. Early Tumor Necrosis Factor Inhibitor Initiation and Chronic Opioid Use in Individuals with Axial Spondyloarthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/early-tumor-necrosis-factor-inhibitor-initiation-and-chronic-opioid-use-in-individuals-with-axial-spondyloarthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/early-tumor-necrosis-factor-inhibitor-initiation-and-chronic-opioid-use-in-individuals-with-axial-spondyloarthritis/