Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The treatment of Rheumatoid Arthritis (RA) has undergone an enormous change in the last two decades with the use of biological Disease Modifying Drugs and targeted therapies (ts/bDMARDs). These drugs are widely used in clinical practice, but we have scarce information about the switching between them in these conditions due to inefficacy. Our objective is to evaluate the incidence rate of switching due to inefficacyas well as the factors associated to switching due to inefficacy.
Methods: We conducted an observational longitudinal retrospective study. Subjects: all patients with recent onset RA diagnosed between January 1st 2007 and December 31st 2015 followed in outpatient clinic at Hospital Clinico San Carlos until January 1st 2022, which used any ts/bDMARDs during at least 3 months. Main outcome: Switching of the ts/bDMARD (suspension and change to a different ts/bDMARD) due to inefficacy. Covariables: sociodemographic, clinical and treatment. Statistical analysis: incidence rates of switching due to inefficacy (IR) per 100 patient-years were estimated using survival techniques with their respective 95% confidence interval [CI]. A multivariate Cox regression analysis was used to evaluate the risk factors of switching due to inefficacy. Results were expressed as HR with their 95% CI.
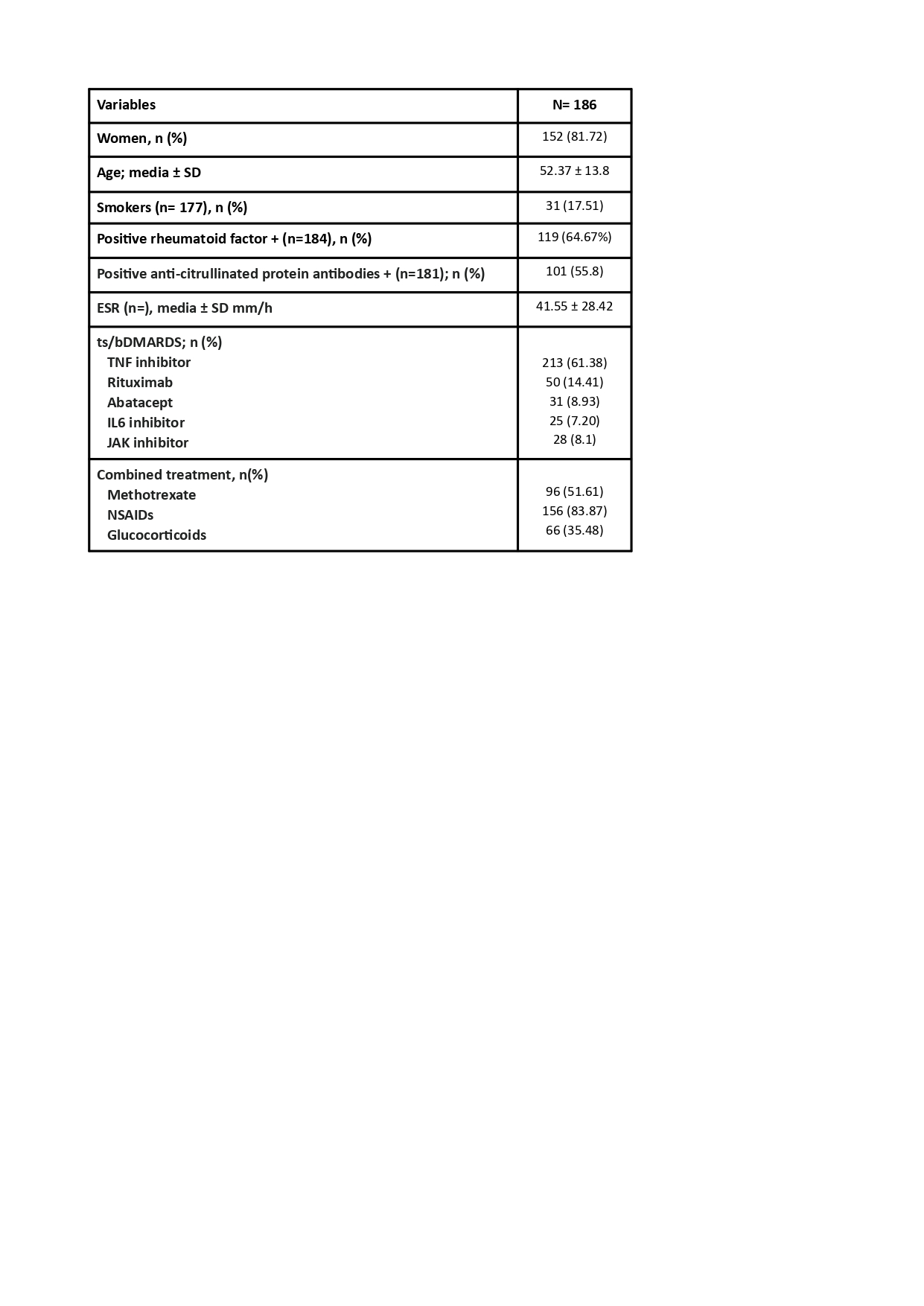
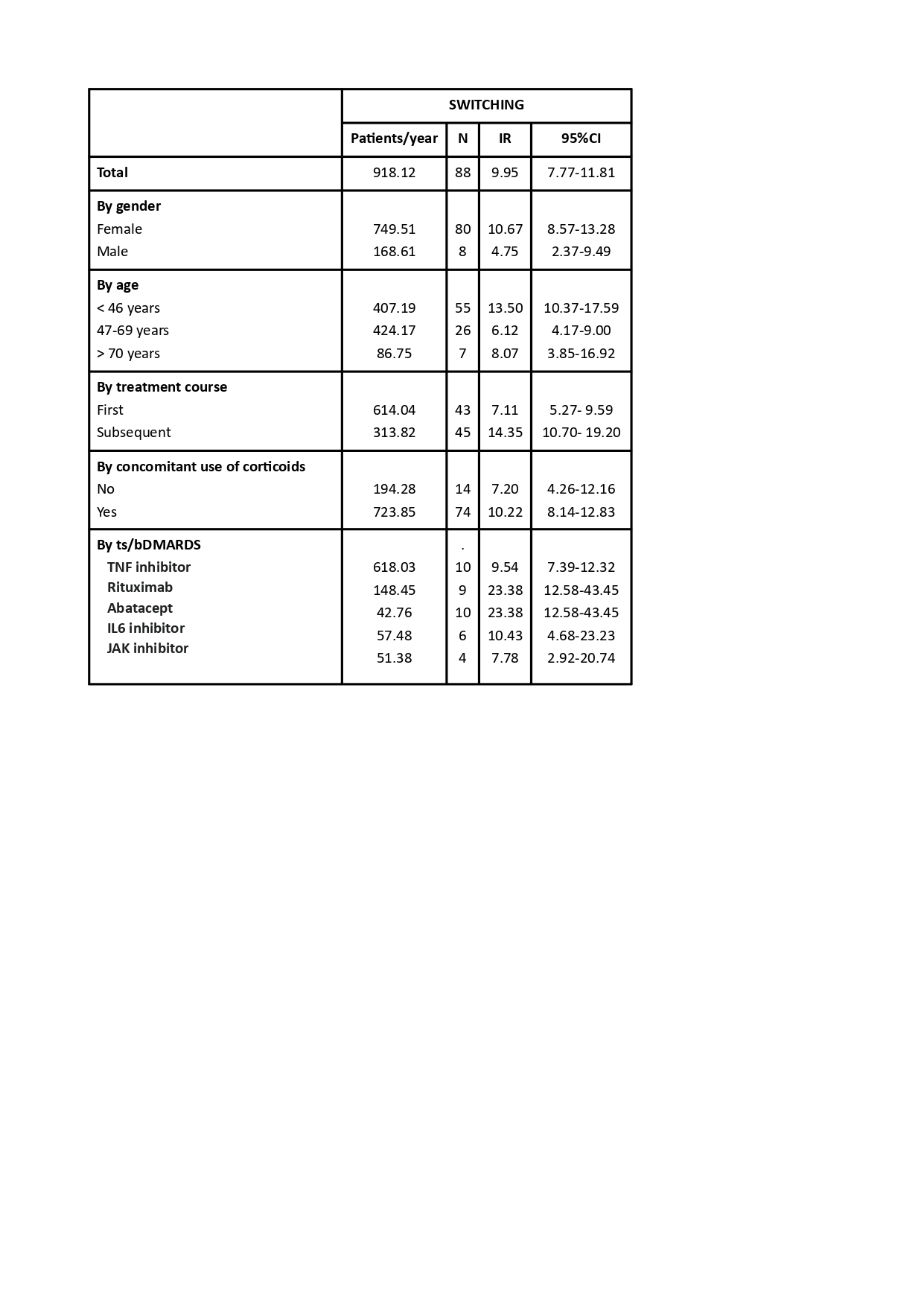
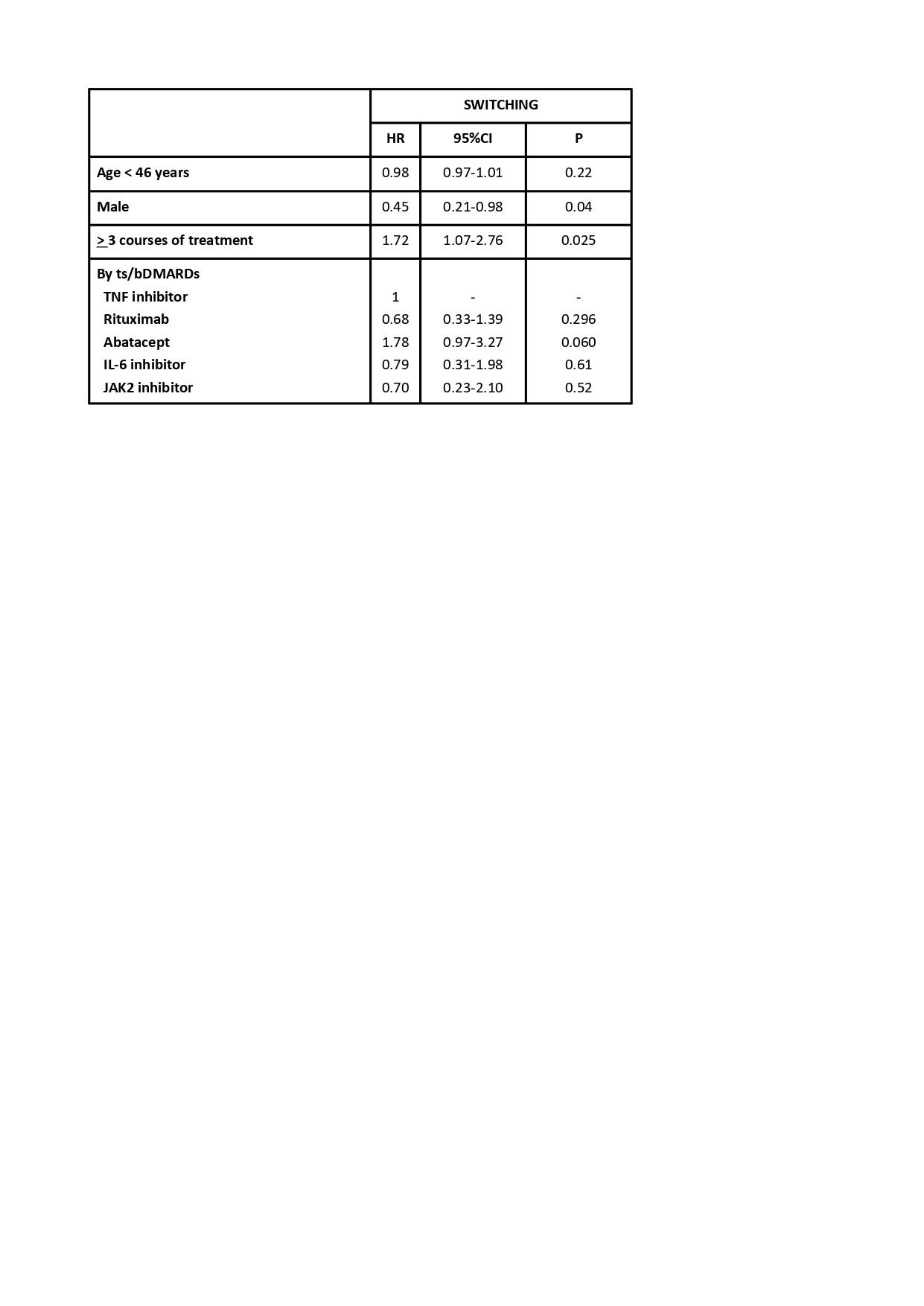
Results: 186 patients were included (927.86 patient-years), 81.72% were women with a mean age of 52.38±13.80. Characteristics at baseline are shown in table 1. The 186 patients received 347 courses of ts/bDMARD treatment of which 88 were switched due to inefficacy (25.36%) with an IR of inefficacy of 9.58 [7.77-11.81]. The most frequent ts/bDMARD group was TNFi (61.38%), specifically Etanercept (21.90%). IRs of switching due to inneficacy are shown in table 1, we found a higher IR in the female sex (IR 10.67 [8.57-13.28]), younger patients (IR 13.50 [10.37-17.59], subsequent courses of treatment (IR 14.34 [10.70-19.20]), with the concomitant use of corticoids (IR 10.22 [8.14-12.83]), and with the use of certain ts/bDMARDs (IR Abatacept 23.38 [12.58-43.45], IR anti-IL6 10.43 [4.68-23.23], IR anti-TNF 9.54 [7.39-12.32], IR JAKi 7.78 [2.92-20.74], IR Rituximab 6.06 [3.15-11.65]). In the multivariate analysis (table 2) we found a higher risk for switching due to inefficacy in patients receiving the third or posterior course of treatment (HR 1.72 [1.07-2.77]) and a tendency in patients in treatment with abatacept compared to anti-TNF (HR 1.79 [0.98-3.28]); the male sex was a protective factor for switching due to inefficacy (HR 0.46 [0.21-0.98]).
Conclusion: Switching of ts/bDMARDs in daily clinical practice due to inefficacy appears with certain regularity (25.36%) with an estimated IR of 9.58. We have found higher switching rates of ts/bDMARDs due to inefficacy in the female sex, younger patients, subsequent courses of treatment, concomitant use of corticoids as well as with some ts/bDMARDs in specific (Abatacept and anti-IL6). Patients receiving the third or posterior course of treatment had a higher risk of switching due to inefficacy meanwhile the male sex acted as a protective factor; treatment with abatacept seemed to have a higher risk to switching due to inefficacy but it did not reach statistical significance.
To cite this abstract in AMA style:
Rodriguez Laguna M, Rosales-Rosado Z, Vadillo-Font C, Otazu-Moudelle J, Pérez Sancristóbal I, Abasolo l. Drug Switching Due to Inefficacy in Rheumatoid Arthritis Patients Treated with Biological and Targeted Therapies. Daily Clinical Experience [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/drug-switching-due-to-inefficacy-in-rheumatoid-arthritis-patients-treated-with-biological-and-targeted-therapies-daily-clinical-experience/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/drug-switching-due-to-inefficacy-in-rheumatoid-arthritis-patients-treated-with-biological-and-targeted-therapies-daily-clinical-experience/