Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Refractory rheumatoid arthritis (reRA) is characterized by an inadequate response to multiple DMARDs. Many factors including environment, comorbidities, sociodemographics, and the treatment itself influence poor treatment response. Accounting for these factors, we sought to quantify any remaining impact of being reRA in modeling the patient global assessment (PtGA) outcome trajectory over time.
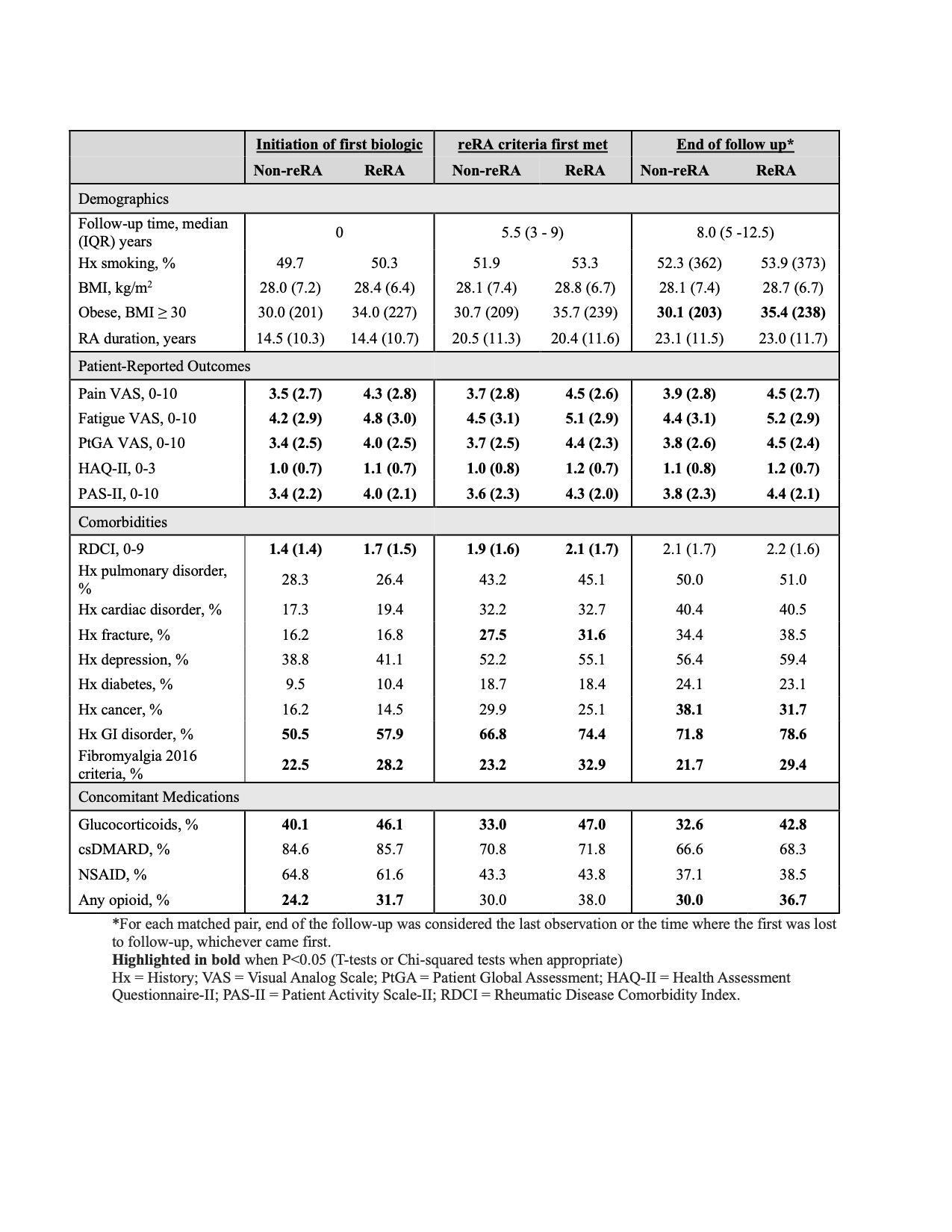
Methods: Participants with RA from the Forward Databank were followed between 1999 and 2019. ReRA was defined as the use of a third advanced therapy with at least one TNFi and a non-TNFi biologic (nTNFi) or JAKi. Participants with RA, stratified into reRA and non-reRA cohorts, were matched based on age, sex, disease duration, and follow-up time to becoming refractory. Patients were followed from initiation of the first biologic until the last observation (each case/control was matched until the first one was lost to follow-up). Demographics, patient-reported outcomes (PROs), comorbidities, and treatment were characterized at several time points during the study, from baseline, when they met the refractory criteria, and at the end of follow-up.
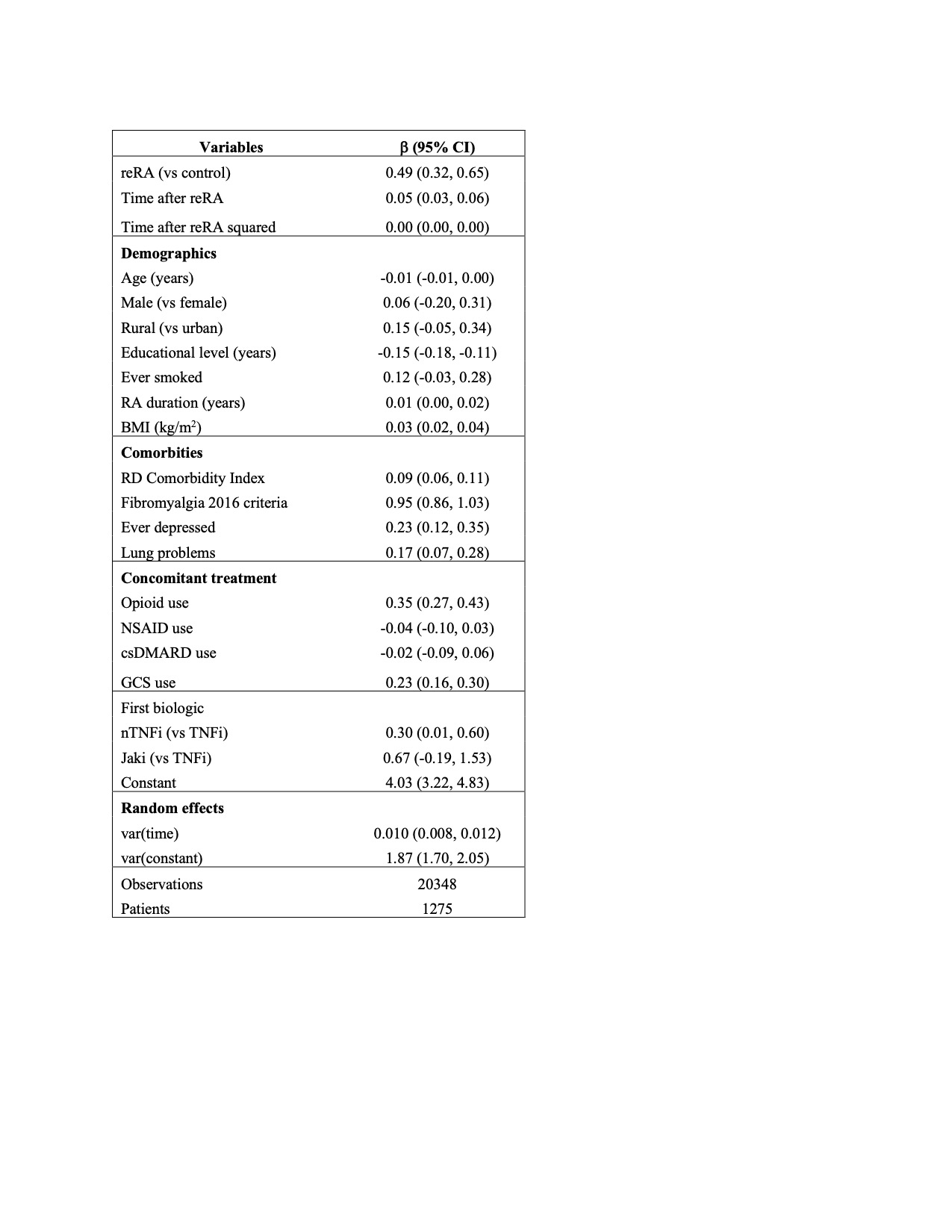
Mixed-effect regression models with random slopes were analyzed using VAS PtGA (rated 0, [VERY WELL], to 10, [VERY POOR]) as the outcome. Akaike information criterion (AIC) was used to identify the best model when adjusting for time, sociodemographic, comorbidities, and treatment (concomitant and initial biologic).
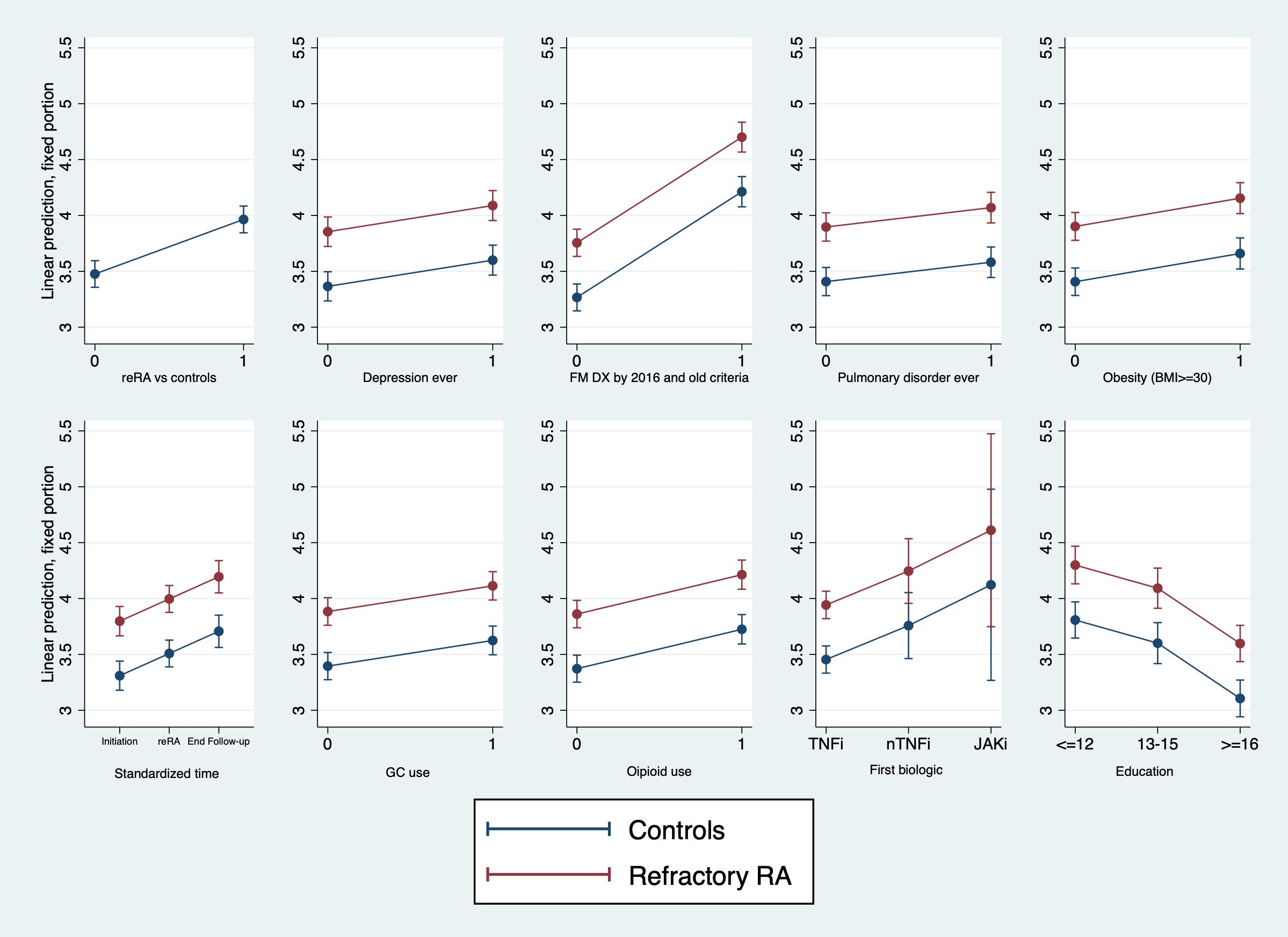
Results: After matching, 1,384 participants were included in the study (692 each). The matched sample was 57 (SD 11) years old, 88% female, 92% white, and had 14 years of education. From the initiation of the first biologic to the last observation, the reRA group was characterized by increased obesity, higher comorbidities, and worse PROs than their controls. These measures also increased over time for both groups (Table 1). The first biologic distribution was: TNFi (89.5%), nTNFi (9.5%), and JAKi (1%). Re-RA vs non-re-RA was associated with an increase of 0.49 in PtGA over follow-up. Similar increases in PtGA were found with concomitant fibromyalgia criteria (0.95), depression (0.23), and lung problems (0.17). Use of opioids (0.35) and glucocorticoids (0.23) was also associated with PtGA increase, as well as starting a nTNFi (0.30) as the first biologic vs TNFi. Education was the only protective variable (-0.15 by school year). Figure 1 presents the predictive margins estimated by the final model.
Conclusion: These findings show that even after accounting for several factors contributing to PtGA over time, reRA status, defined by only treatment use, is still highly associated with PtGA. This shows the possible value of having a reRA definition agnostic to disease activity as these 2 groups had distinct trajectories over time. Future work is also needed to identify and quantify the impact of the factors contributing to worse trajectories of PtGA score and other outcomes for those who are refractory compared to their controls.
To cite this abstract in AMA style:
Pedro S, Wipfler K, Sbarigia U, Zazzetti F, Sheahan A, Katz P, Michaud K. Does Refractory Rheumatoid Arthritis Status Matter in Modeling Patient Global Assessment Trajectories over 20 Years in a Large US Registry? [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/does-refractory-rheumatoid-arthritis-status-matter-in-modeling-patient-global-assessment-trajectories-over-20-years-in-a-large-us-registry/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/does-refractory-rheumatoid-arthritis-status-matter-in-modeling-patient-global-assessment-trajectories-over-20-years-in-a-large-us-registry/