Session Information
Date: Sunday, November 7, 2021
Title: Measures & Measurement of Healthcare Quality Poster (0623–0659)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Quality of care (QOC) as measured by quality indicators (QIs) decreases damage accrual in SLE long term. We aimed to assess if high QOC in SLE results prospectively in improved outcomes, specifically patient reported quality of life (QOL) and non-routine health care utilization (HCU).
Methods: 140 consecutive patients meeting 1997 ACR classification criteria for SLE were recruited from the Rheumatology clinic at an academic center. Self-report questionnaires collected information on QOC and QOL (using the disease-specific tool LupusPRO, which assesses both health-related (HR) QOL and non (N)HRQOL) at baseline. Receipt of QIs was confirmed using chart review. Data on demographics, socio-economic and disease characteristics were collected. Disease activity and damage were measured using Safety of Estrogens in Lupus Erythematosus National Assessment (SELENA)- SLEDAI and SLICC-ACR damage index (SDI). Follow up QOL and HCU (routine: rheumatology, primary care physician (PCP) visits and non-routine: ER visits and hospitalizations) were collected prospectively at 6 months. High QOC was defined as those meeting ≥80% of the eligible QIs. Co-variates of high QOC were assessed. Univariate regression analyses were performed with QOC (continuous variable) and high QOC (binary variable) as independent variables and HRQOL and NHRQOL as the dependent variables at baseline and follow up. Multivariable regression models were adjusted for age, gender, public insurance, disease activity, damage, disease duration, fibromyalgia and Charlson comorbidity index. HCU was also included in the multivariate models for QOL at follow up. Similarly, univariate and multivariate regression analyses were performed to evaluate QOC (and high QOC) as the predictors of non-routine HCU and disease activity at follow up. P-value of ≤0.05 was significant.
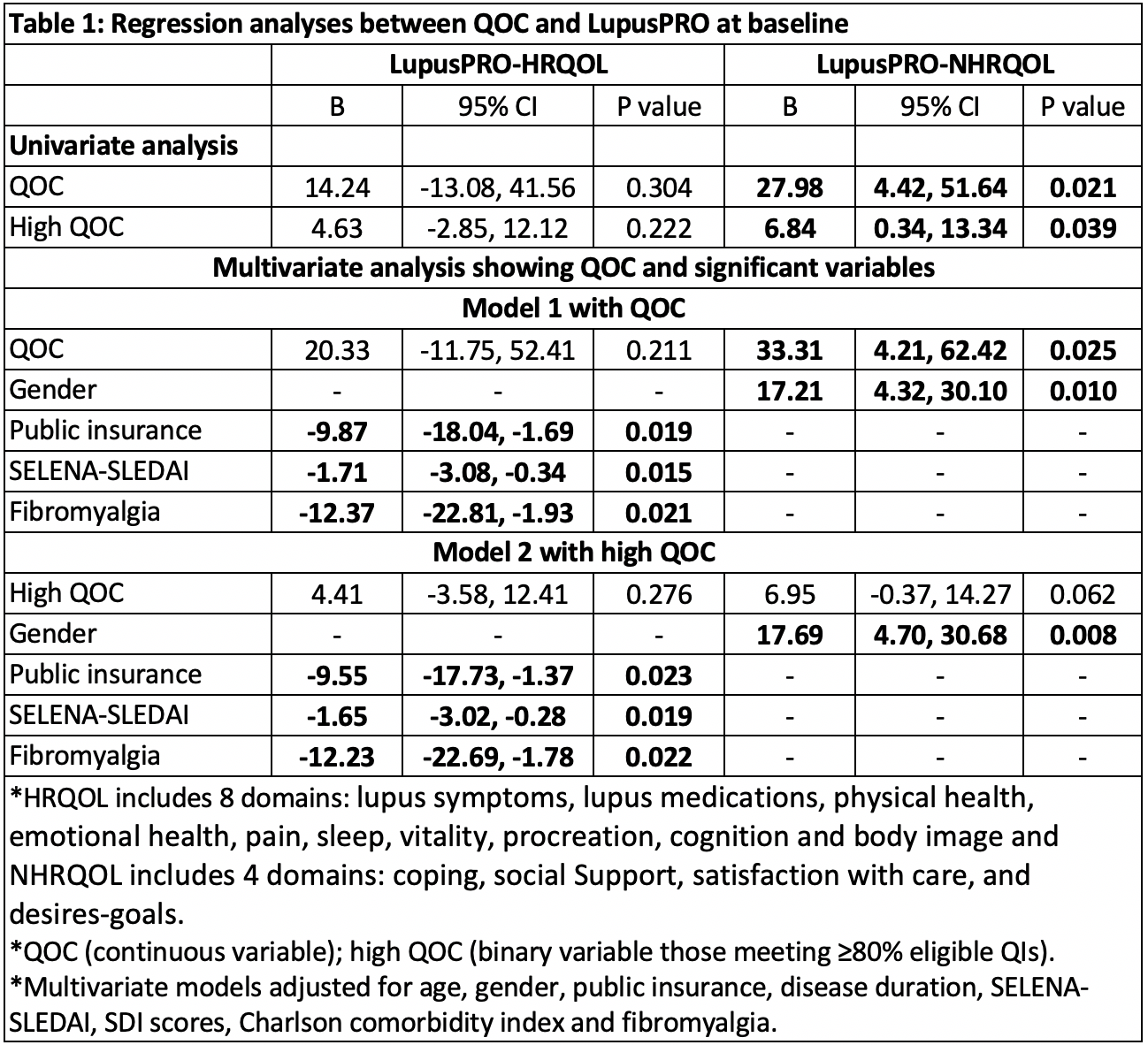
Results: Baseline and follow up data on 140 and 94 patients respectively were analyzed. Mean (SD) age was 45.3 (13.5) years, with 88.6% females. Mean (SD) cumulative performance rate (QOC) was 78.6 (13.4) with 52% patients in the high QOC group. Older age and longer disease duration were the only significant predictors of high QOC. On univariate analysis QOC (and high QOC) were associated with better NHRQOL at baseline but not with HRQOL (Table 1). QOC remained a significant correlate of baseline NHRQOL, even after adjusting for co-variates. Of all the NHRQOL domains, high QOC was associated with better treatment satisfaction.
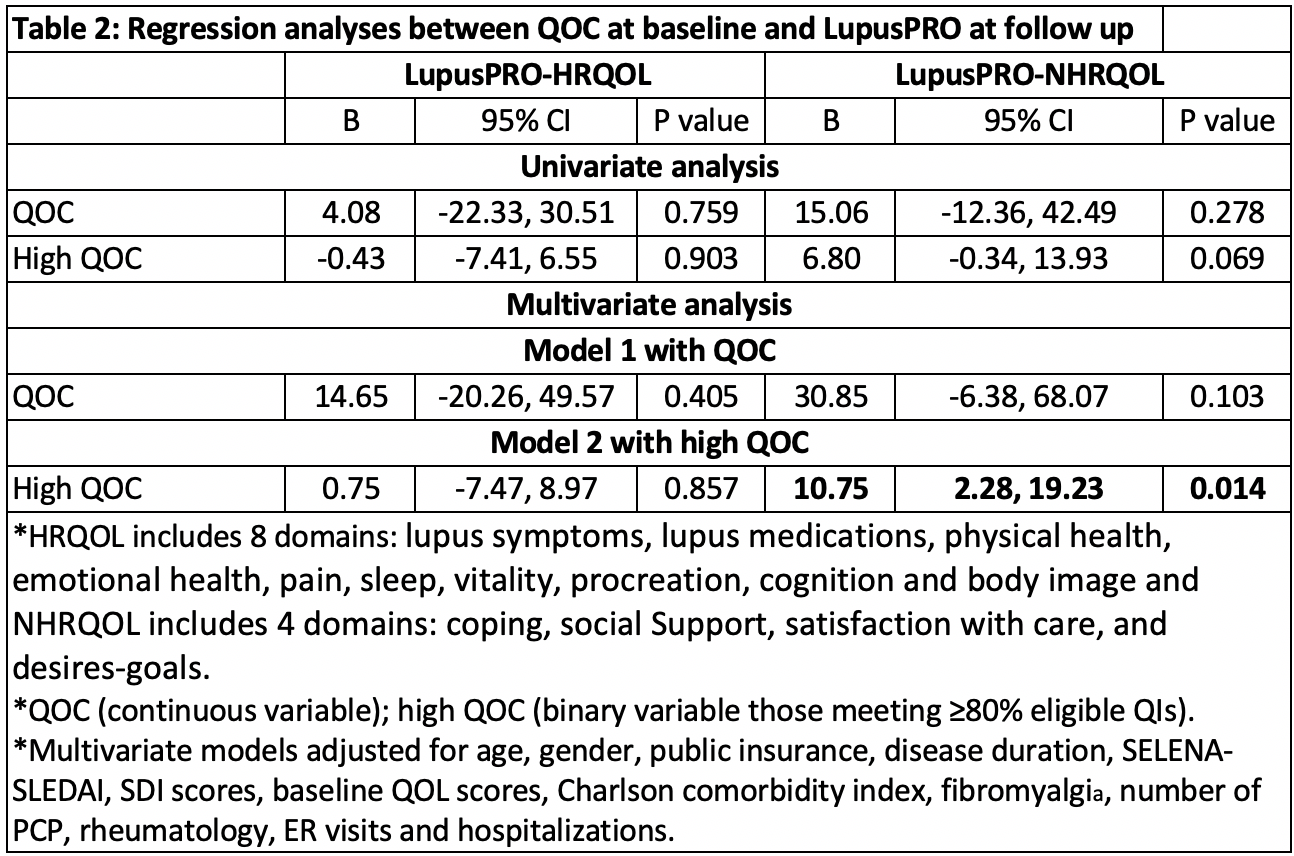
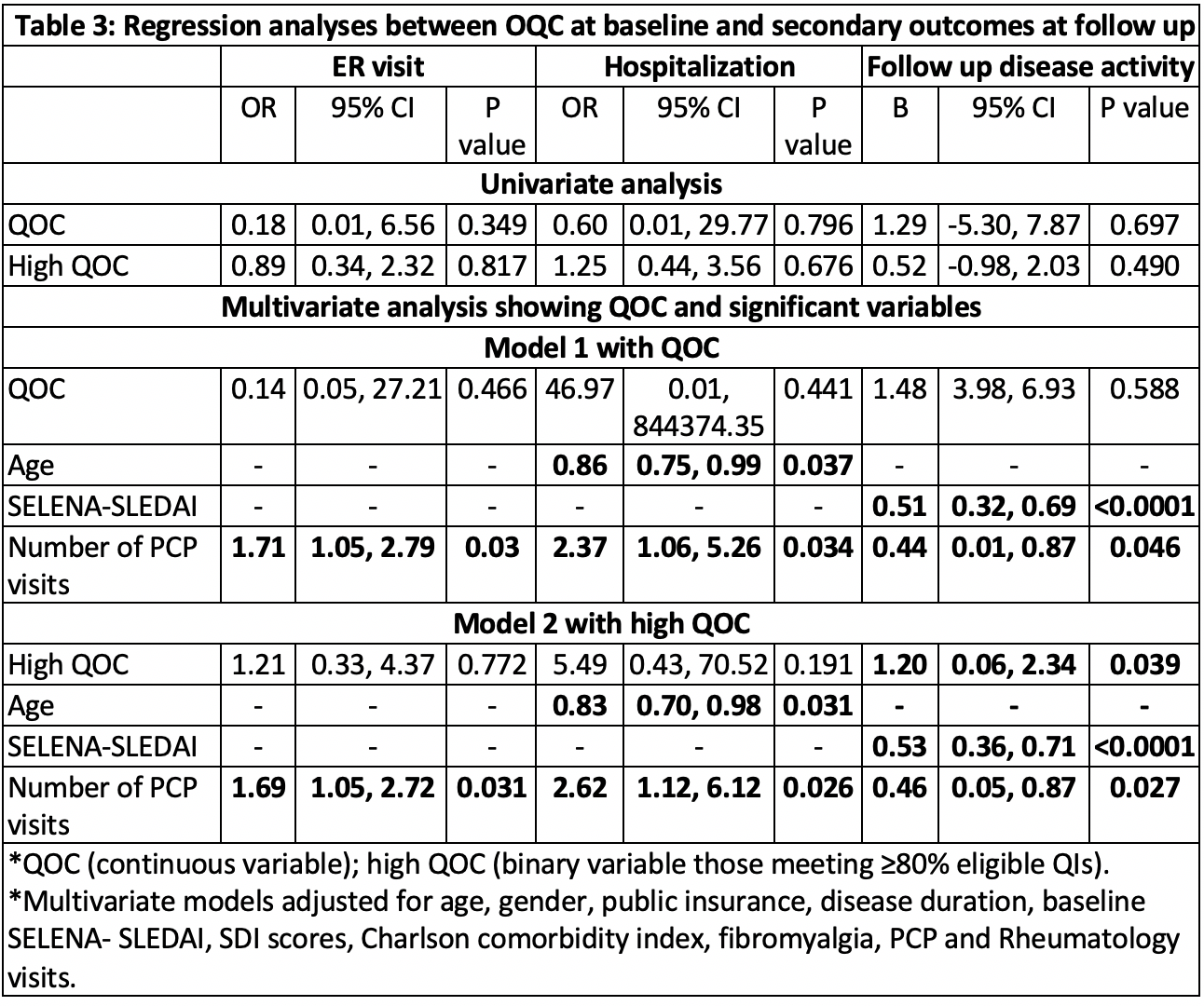
QOC (or high QOC) was not predictive of HRQOL or NHRQOL at follow up on univariate analysis; however, high QOC at baseline predicted better NHRQOL at follow up on multivariate analysis (Table 2). QOC was not associated with non-routine HCU at follow up (Table 3). High QOC, baseline disease activity and number of PCP visits were significantly associated with higher disease activity at follow up on multivariate analysis.
Conclusion: Higher QOC predicted better NHRQOL by directly impacting treatment satisfaction, which has been noted to influence health behaviors and improve adherence and outcomes in SLE patients. Higher QOC was not associated with HRQOL, ER visits, hospitalizations, or improvement in disease activity at follow up.
To cite this abstract in AMA style:
Arora S, Block J, Nika A, Sequeira W, Katz P, Jolly M. Does Higher Quality of Care in SLE Translate to Better Patient Outcomes? [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/does-higher-quality-of-care-in-sle-translate-to-better-patient-outcomes/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/does-higher-quality-of-care-in-sle-translate-to-better-patient-outcomes/