Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Knee osteoarthritis (KOA) is a major cause of disability worldwide, particularly impacting the elderly and obese population. Radiographic trabecular bone texture (TBT) is demonstrated as a promising biomarker for predicting KOA progression. However, integrating MRI biomarkers with TBT from the Osteoarthritis Initiative (OAI) cohort remains underexplored. Our study aimed to assess whether associating MRI biomarkers with TBT biomarkers could enhance the predictive performance of models for KOA progression
Methods: From the OAI database, 1812 patients were selected, meeting predefined criteria (outlined in Figure 1), including knees with Kellgren-Lawrence (KL) scores of 2 or 3, availability of baseline and 48-month follow-up medial joint space narrowing (JSNM) scores, and availability of baseline clinical and MRI parameters. Clinical parameters included sex, age, body mass index, pain, and race. MRI parameters investigated included quantitative measures such as cartilage thickness (CartTh) and area (CartA), as well as semi-quantitative assessments such as meniscal tears (MTs), bone marrow lesions (BMLs) and anterior cruciate ligament (ACL) damage. Cases were defined as those with increased JSNM within 48 months. A prediction model using TBT biomarkers associated with the aforementioned clinical covariates and other radiological scores (KL and JSNM) served as a reference model. Other prediction models were created by incorporating combinations of the aforementioned MRI biomarkers. Performance analyses employed logistic regression with 10-fold cross-validation repeated 300 times. The area under the ROC curve (AUC) served as the primary metric, and balanced accuracy (BACC), positive predictive value (PPV) and negative predictive value (NPV) as secondary metrics.
Results: Among the analyzed knees, 981, 763, 762 and 553 had CartTh and CartArea, BMLs, MTs, and ACL data, respectively. The characteristics of these datasets are presented in Table 1. Performance results, as shown in Table 2, demonstrated slightly higher AUC scores, but not statistically significant, when adding one or a combination of MRI parameters to the reference model. For example, when adding all 5 MRI biomarkers, the model slightly improved (AUC=0.71, p-value=0.7), compared to the reference model (AUC=0.70). Comparable results were observed for secondary metrics.
Conclusion: Integrating certain MRI-based biomarkers (CartTh, CartA, MTs, BMLs and ACL data) into a reference XR-based model using TBT biomarkers associated with clinical and radiographic biomarkers did not show evidence of improving the performance in predicting radiographic KOA progression.
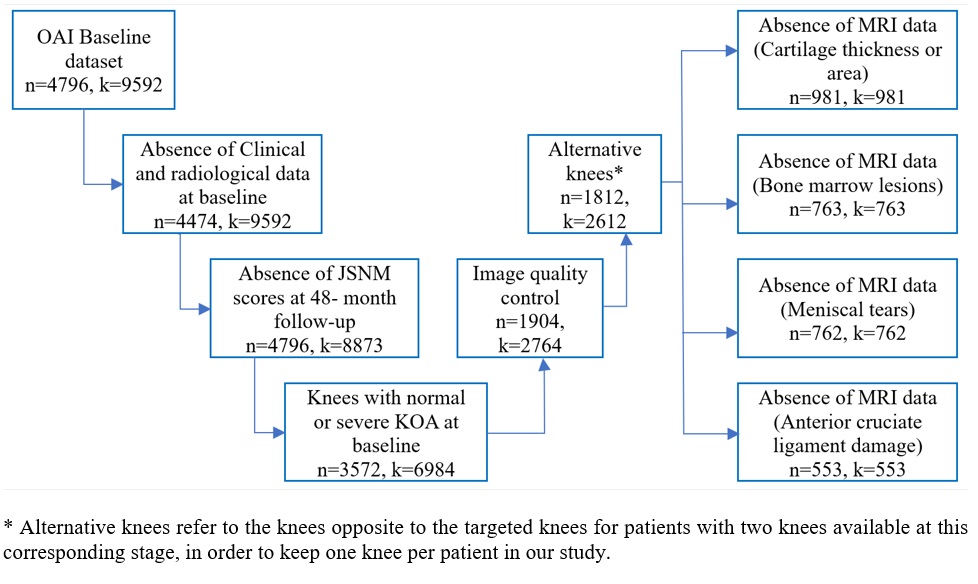 Figure 1: Diagram of the data selection process followed in the study.
Figure 1: Diagram of the data selection process followed in the study.
.jpg) Table 1: Characteristics of the dataset included in the study.
Table 1: Characteristics of the dataset included in the study.
.jpg) Table 2: Performance results of the prediction models evaluated in the study.
Table 2: Performance results of the prediction models evaluated in the study.
To cite this abstract in AMA style:
Almhdie-Imjabbar A, Daroussi S, Herrera D, Toumi H, Lespessailles E. Does Combining Standard MRI-Based Scores with Radiographic Trabecular Bone Texture Biomarkers Improve Predictive Performance for Radiographic Knee Osteoarthritis Progression? [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/does-combining-standard-mri-based-scores-with-radiographic-trabecular-bone-texture-biomarkers-improve-predictive-performance-for-radiographic-knee-osteoarthritis-progression/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/does-combining-standard-mri-based-scores-with-radiographic-trabecular-bone-texture-biomarkers-improve-predictive-performance-for-radiographic-knee-osteoarthritis-progression/
