Session Information
Session Type: Breakout Session
Session Time: 5:10PM-5:40PM
Background/Purpose: Sialadenitis is a common distinguishing manifestation of Childhood Sjogrens Disease (cSD). We have previously reported a surprisingly high rate of Childhood Sjogrens Disease (cSD) patients who presented with recurrent parotitis. For this reason, we created a pediatric multidisciplinary otolaryngology/rheumatology clinic (PMORC) which was founded in December 2019 at the University of Utah. Currently little is known about cSD and there is no widely accepted classification criteria. The aim of the study was to analyze clinical characteristics of patients with cSD and evaluate how many patients currently met 3 proposed but not widely accepted or validated classification criteria for children in this clinic.
Methods: Retrospective analysis of patients seen in this PMORC between December 2019 and July 2022 presenting with chronic sialadenitis was performed. Patients were included in the cSD group if diagnosed with cSD by a pediatric rheumatologist. Systematic evaluation of demographic information, clinical symptoms, and lab/biopsy/imaging results were collected. Patients were evaluated to see if they met the 2016 ACR-EULAR criteria, 1999 Japanese criteria, and proposed Bartunkova criteria for cSD. The framework of this PMORC included a new patient evaluation, a minor salivary gland biopsy and therapeutic sialendoscopy with triamcinolone acetonide injection, and follow up.
Results: 27 patients presented to the PMORC and 14 (51.9%) were diagnosed with cSD. 7 (50%) patients were female with a median age of symptom onset of 6.5 (1-15) years. 14 (100%) patients had parotid swelling, 4 (28.6%) had joint pain, 9 (64.3%) had dry eyes symptoms, 10 (71.4%) had dry mouth symptoms, 2 (14.3%) had fevers. 13 (92.9%) of the patients showed histologic proof of focal lymphocytic infiltration. 5 (35.7%) patients were positive for anti-SSA, anti-SSB and/or ANA autoantibodies.
13 cSD patients and 3 non-cSD patients had focal lymphocytic infiltrate on biopsy (p=0.00023), 13 cSD and 8 non-cSD patients had abnormal ultrasounds (p=0.050), 9 cSD and 2 non-cSD patients had symptoms of dry eyes (p=0.0098), and 6 cSD and 0 non-cSD patients received a focus score of greater than one on biopsy (p=0.0074).
2 patients (14.32%) met the 2016 ACR-EULAR criteria and 2 (14.32%) met the Japanese criteria based on a positive biopsy score and positive serology.7 (50%) cSD patients met the pediatric Bartunkova criteria. Additionally, 1 patient in the non-cSD cohort met the Bartunkova criteria.
Conclusion: Given the variable features of cSD compared to adult SD, there is a need for a validated pediatric criterion. The 2016 ACR-EULAR criteria and 1999 Japanese criteria were not sufficient in identifying cSD in our clinic. Additionally, Bartunkovas proposed cSD criteria only diagnosed 50% of our cohort that received a clinical diagnosis of cSD in our clinic. Therefore, providers should have a high index of suspicion of cSD for children presenting with recurrent sialadenitis.
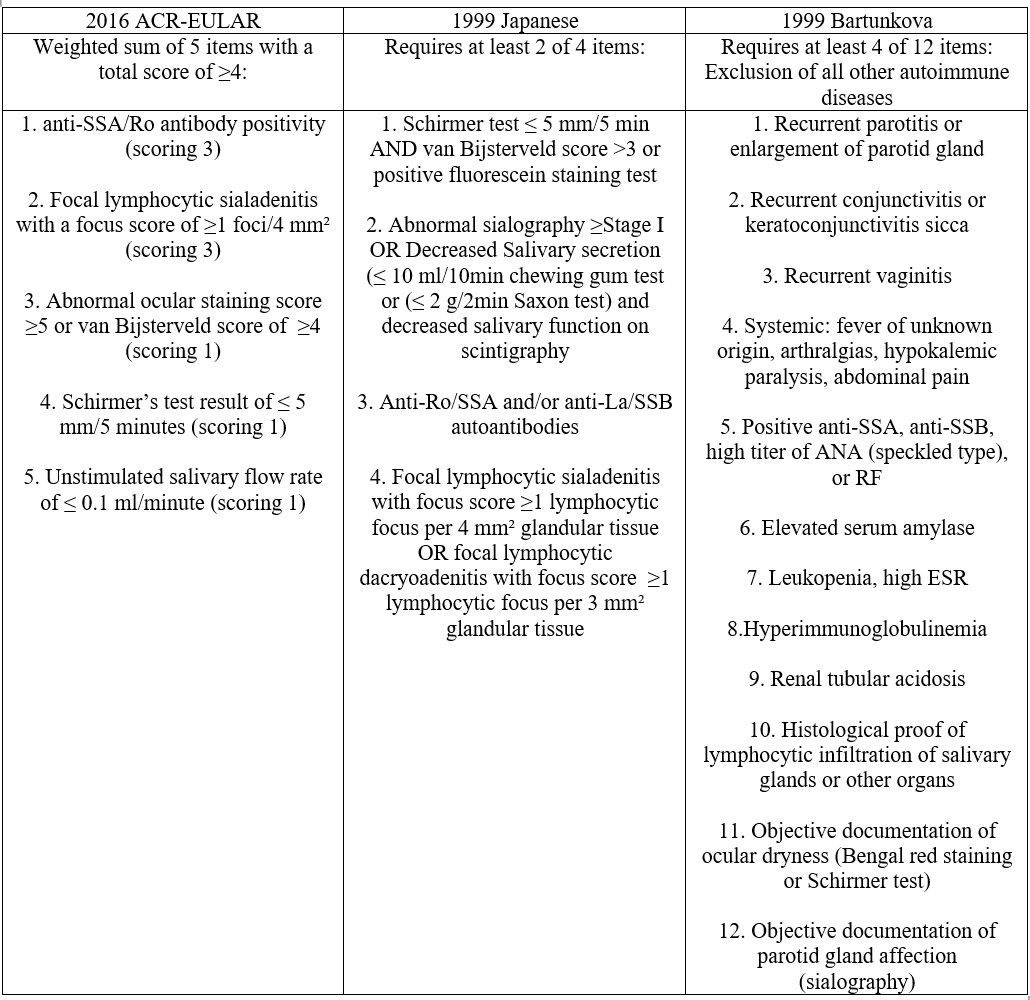 Criteria for Classification of SD
Criteria for Classification of SD
 Bartunkova Criteria – cSD Cohort
Bartunkova Criteria – cSD Cohort
 Bartunkova Criteria – Entire Cohort
Bartunkova Criteria – Entire Cohort
To cite this abstract in AMA style:
Holley A, Stern S. Distinguishing Childhood Sjogren’s Disease in Patients Presenting with Recurrent Sialadenitis in a Multidisciplinary Clinic [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/distinguishing-childhood-sjogrens-disease-in-patients-presenting-with-recurrent-sialadenitis-in-a-multidisciplinary-clinic/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/distinguishing-childhood-sjogrens-disease-in-patients-presenting-with-recurrent-sialadenitis-in-a-multidisciplinary-clinic/
