Session Information
Title: B cell Biology and Targets in Autoimmune Disease: Systemic Lupus Erythematosus and Related Diseases
Session Type: Abstract Submissions (ACR)
Background/Purpose
Monoclonal antibodies (mAbs) targeting B cell antigens CD20 and CD22 are used to treat patients with SLE either in the clinic or in clinical trials whilst anti-CD19mAbs have been studied in vitro. The main mechanisms of action of these mAbs are depletion and immunomodulation. Internalisation of antigens bound to mAbs is key to immunomodulatory action whereas retention of mAbs on cell surface evokes immune effector mechanisms triggering depletion.
Methods
We studied internalisation of anti-CD19 mAb (RFB9), type1 anti-CD20 mAb (Rituximab), type2 anti-CD20mAb (BHH2, glycosylated GA101), anti-CD22 mAb (4KB128) and anti-CD38mAb (AT13/5h) in 11 patients with SLE. Internalisation of mAbs was assessed using the surface fluorescence-quenching assay on isolated B cells. We used AT10, a mAb against the Fcgamma receptor II (CD32), to assess whether it regulated internalisation of mAbs. Isolated B cells were incubated with mAbs +/- AT10. Paired “t’ test or Mann-Whitney U test was used to compare groups, as appropriate.
Results
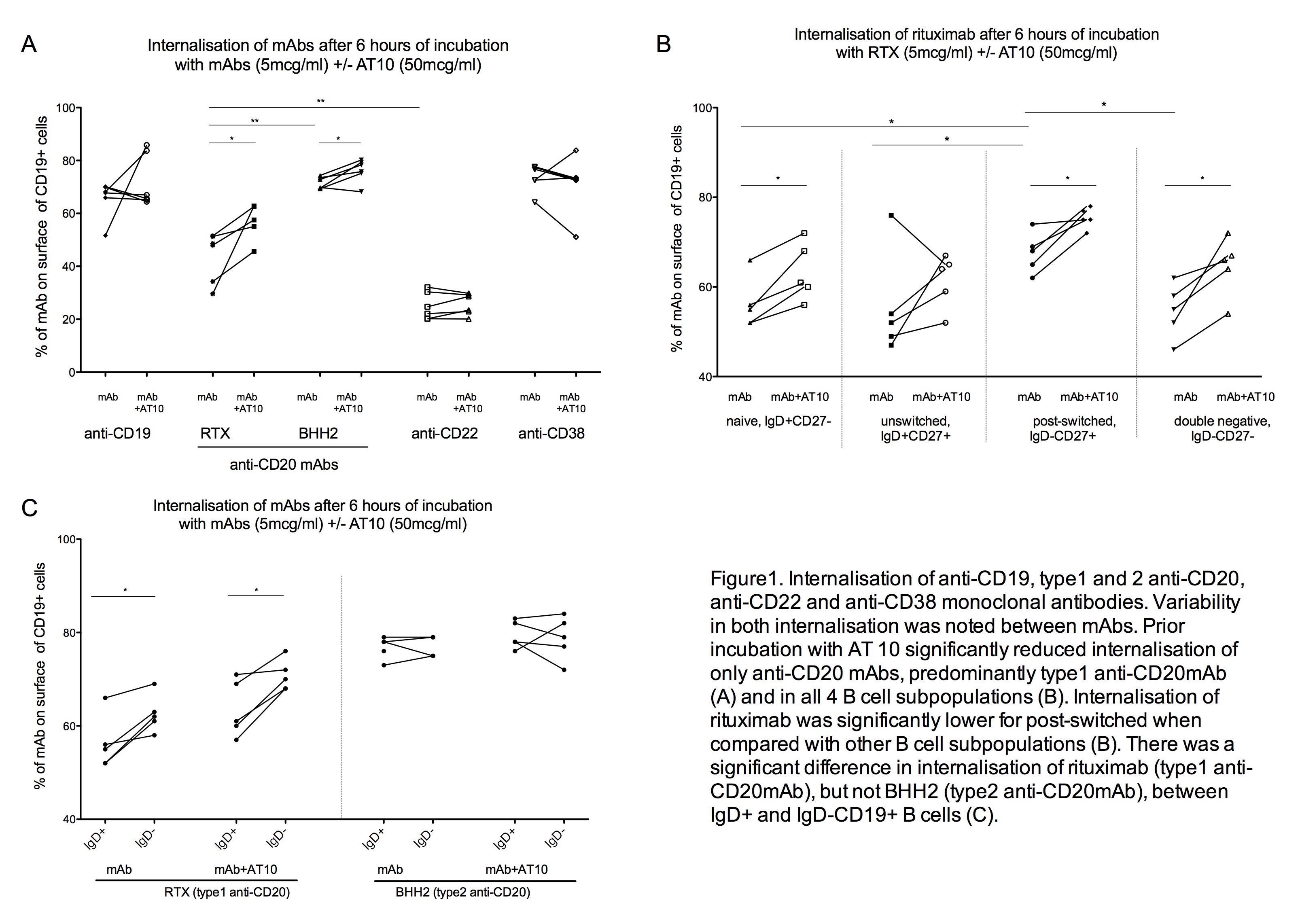
We performed surface fluorescence-quenching assay in 11 patients with SLE, assessed internalisation of mAbs after 6 hours of incubation with mAbs (5 mcg/mL), with or without prior incubation with AT10 (50mcg/mL) in 6/11. The median % of surface accessible mAbs was 68, 48, 71, 23 and 76 for anti-CD19, type1 anti-CD20, type2 anti-CD20, anti-CD22 and anti-CD38, respectively. However, prior incubation with AT10 significantly reduced internalisation of onlyanti-CD20 antibodies, a mean reduction of 12% and 4% for type1 and type2, respectively (Figure 1.A). A remarkable variability between patients in both the extent of internalisation and reduction in internalisation with AT10 was noted for rituximab, but not BHH2 (type2 anti-CD20mAb).
Internalisation of type1 and 2 anti-CD20mAbs in B cell subpopulations Internalisation of type1, but not type2, anti-CD20mAbs was significantly lower for post-switched cells (IgD-CD27+) when compared with other B cell subpopulations (na•ve, IgD+CD27+; unswitched, IgD+CD27+; and double negative, IgD-CD27-) (p<0.05 for all). AT10 reduced internalisation of type1, but not type2, mAb in all B cell subpopulations (Figure 1.B). Internalisation was also 9% greater for IgD+ vs IgD- Bcells (p<0.005) suggesting a role for IgD in internalisation of mAbs, probably in synergy with Fcgamma receptor IIb (as B cells predominantly express the inhibitory Fcgamma receptor IIb)(Figure 1.C).
Conclusion
Disparity in internalisation of mAbs occurs, with a high rate for anti-CD22mAb, probably related to its high physiological rate of endocytosis and less so for type1 anti-CD20 mAbs. Disparity between B cell subpopulations in internalisation of type 1 anti-CD20 mAbs may occur due to differential expression of IgD and Fcgamma receptor IIb. Therefore, internalisation of mAbs poses important therapeutic implications for targeted therapy in SLE.
Disclosure:
V. Reddy,
None;
G. Cambridge,
None;
D. A. Isenberg,
None;
M. Cragg,
None;
M. J. Leandro,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/disparity-in-internalisation-of-monoclonal-antibodies-targeting-b-cell-antigens-and-regulation-by-fc-gamma-receptor-iib-implications-for-targeted-therapy-in-sle/