Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Disease progression in systemic sclerosis (SSc) is characterized by severe and early progression in anti-topoisomerase (ATA) positive diffuse cutaneous patients and typically involves lung and skin. Disease progression in anti-centromere (ACA) patients is also frequently present, but more often consists of cardiac progression and happens typically not early but any time during the course of disease. We therefore hypothesize that disease progression in ACA-positive patients is driven by different factors than disease progression in ATA-positive patients. The aim of this study is to identify baseline characteristics that predict disease progression in ACA-positive SSc patients.
Methods: SSc patients fulfilling ACR/EULAR 2013 criteria were included form the Leiden CCISS cohort. Disease progression was defined as disease progression in one or more organ domains (including skin involvement, heart involvement, interstitial lung disease (ILD), pulmonary arterial hypertension (PAH), renal involvement, myositis and gastro-intestinal involvement) or death. To identify possible baseline predictors for disease progression univariable and multivariable logistic regression with adjustment for age, sex and immunosuppressive use at baseline was performed.
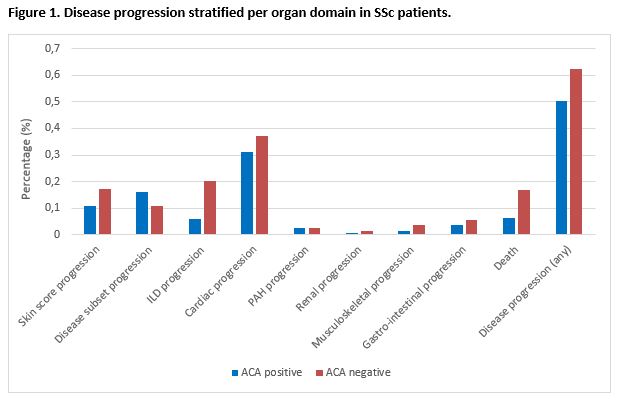
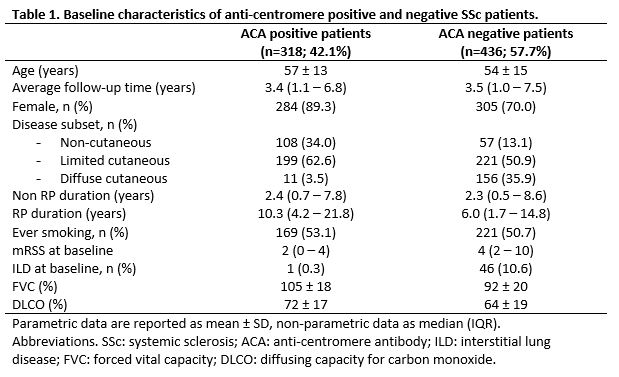
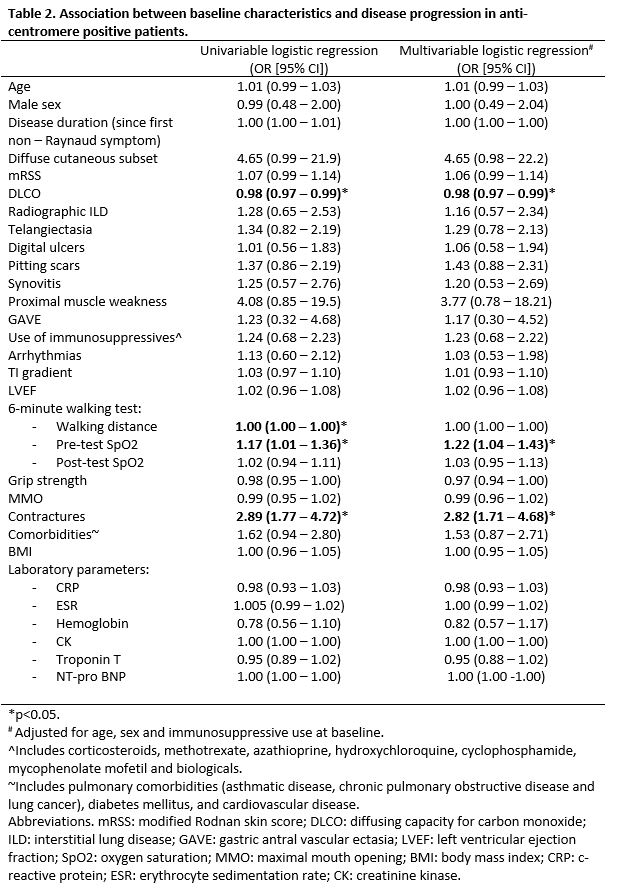
Results: In total 754 patients were included, with a median follow-up of 3.4 (1.1–7.1) years. Of 318 ACA-positive patients 160 (50%) suffered from disease progression during follow-up, compared to 62% in ACA-negative patients. In ACA-positive patients, cardiac progression occurred most frequently (31%), followed by disease subset progression (16%) and skin score progression (11%), whereas in ACA-negative patients disease progression most frequently involved cardiac progression (37%), ILD progression (20%) and skin score progression (17%) (Figure 1). In univariable analysis diffusing capacity for carbon monoxide (DLCO), 6 minute walking distance, oxygen saturation at rest and presence of contractures were significantly associated with disease progression in ACA-positive patients, while for the total group skin score, diffuse cutaneous subset, hemoglobin, and presence of radiographic ILD, pitting scars and friction rubs were predictive as well. In multivariable analysis DLCO percentage (OR 0.98 [0.97-0.99]), oxygen saturation at rest (OR 1.22 [1.04-1.43]) and contractures (OR 2.82 [1.71–4.68]) were significantly associated with disease progression.
Conclusion: Our study confirms that disease progression is substantial in ACA-positive patients. The baseline characteristics most predictive for progression in ACA-positive patients include DLCO percentage, oxygen saturation at rest and contractures, which were clearly different from predictors for the complete SSc group and should be taken into account in risk stratification in clinical practice. Our results underline the hypothesis that disease progression is driven by different factors in ACA-positive patients; further in-depth studies are warranted.
To cite this abstract in AMA style:
Hoekstra E, Ahmed S, Ueckert D, Ajmone Marsan N, Kiès P, Ninaber M, Heuvers M, Geelhoed M, Huizinga T, de Vries-Bouwstra J. Disease Progression in Anti-Centromere Positive Systemic Sclerosis Patients [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/disease-progression-in-anti-centromere-positive-systemic-sclerosis-patients/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/disease-progression-in-anti-centromere-positive-systemic-sclerosis-patients/