Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Although severity of skin involvement and change in skin thickness over time vary substantially between patients with diffuse cutaneous systemic sclerosis (dcSSc), for the majority of patients, skin tends to improve over time. We were interested in determining the effect of autoantibodies on the patterns of change in skin thickness over time in patients with dcSSc.
Methods:
Subjects with confirmed diagnosis of dcSSc and at least one modified Rodnan skin score assessment were included. Linear mixed models were used to assess association between changes in mRss over time and autoantibody specificities.
Results:
In total, 572 dcSSc patients were included. Of those, 127 (22.2%) were male and mean±SD age at disease onset was 44.5±13.7 years. The most common scleroderma-specific antibodies were anti-topoisomerase I (ATA), present in 174 (30.4%) and anti-RNA polymerase (ARA) in 153 (26.8%) of the subjects. Anti-U3RNP was found in 39 (6.8%), anti-PmScl in 28 (4.9%) and ACA in 17 (3%). A substantial proportion of the cohort was ANA+, but ENA- (n=99, 17.3%). Other antibody specificities included anti-nRNP, SL, Ku, Jo1, Ro, PL7, hnRNP and Sm. In 24 subjects (4.2%) ANA was negative. Three or more mRss assessments were available for 72.2% (n=413). For 66.4% of the patients (n=380), first mRss assessment was made within 3 years from disease onset.
For the cohort as a whole, the average mRss at 12 months from disease onset was estimated to be 23.5 (SD 9.4; 95%CI 22.6, 24.5) and this gradually declined following a non-linear trajectory (mRss=23.5-2.3*years+0.1*years^2-0.002*years^3, p<0.001 for all parameters). Thus skin improvement was greater in earlier disease (average drop in mRss was 2.2 between years 1 and 2, compared to 1.58 between years 4 and 5, and 0.8 between years 9 and 10, for example). There was a moderately strong, negative association between mRss at 1 year and drop in mRss over time (correlation coefficient=-0.62), suggesting that higher initial skin scores are associated with greater subsequent improvement.
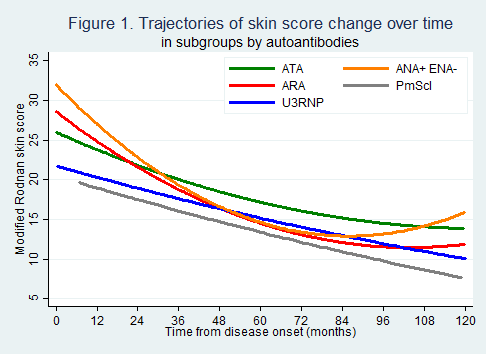
Focusing on the first 10 years of disease, autoantibodies showed significant association with both baseline mRss and changes in mRss over time (Figure 1). At 1 year from disease onset, highest average mRss (27.0) was observed in ANA+ ENA- patients. Compared to those, mRss in ARA+ patients was 24.9, p=0.166; in ATA+ 23.8, p=0.043; in anti-U3RNP+ 20.3, p=0.008 and in anti-PmScl+ 19, p=0.009. Over subsequent years, the greatest improvement was observed in ANA+ ENA- and ARA+ patients with respective drop in mRss of 4.2 and 3.3 between year 1 and 2, compared to 2 in ATA+ patients (p<0.005) and 1.4 in anti-U3RNP+ (p<0.020).
Conclusion:
Skin score change is significantly associated with autoantibody specificity and disease duration. While mRss can be much higher in ARA+ and ANA+ENA- patients compared to other antibodies, those patients experience the greatest improvement over time.
To cite this abstract in AMA style:
Nihtyanova SI, Sari A, Ong VH, Denton CP. Disease Duration and Autoantibodies Predict Distinct Skin Score Trajectories in Diffuse Cutaneous Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/disease-duration-and-autoantibodies-predict-distinct-skin-score-trajectories-in-diffuse-cutaneous-systemic-sclerosis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/disease-duration-and-autoantibodies-predict-distinct-skin-score-trajectories-in-diffuse-cutaneous-systemic-sclerosis/