Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Sleep disorders are common among patients with inflammatory arthritis (IA) and have probably bilateral influence on disease activity and quality of life. Pathomechanism of sleep impairment is complex and may differ among patients with RA, axSpA and PsA. Our research offers a novel direct comparison of sleep quality and risk factors for poor sleep in these three most common forms of IA.
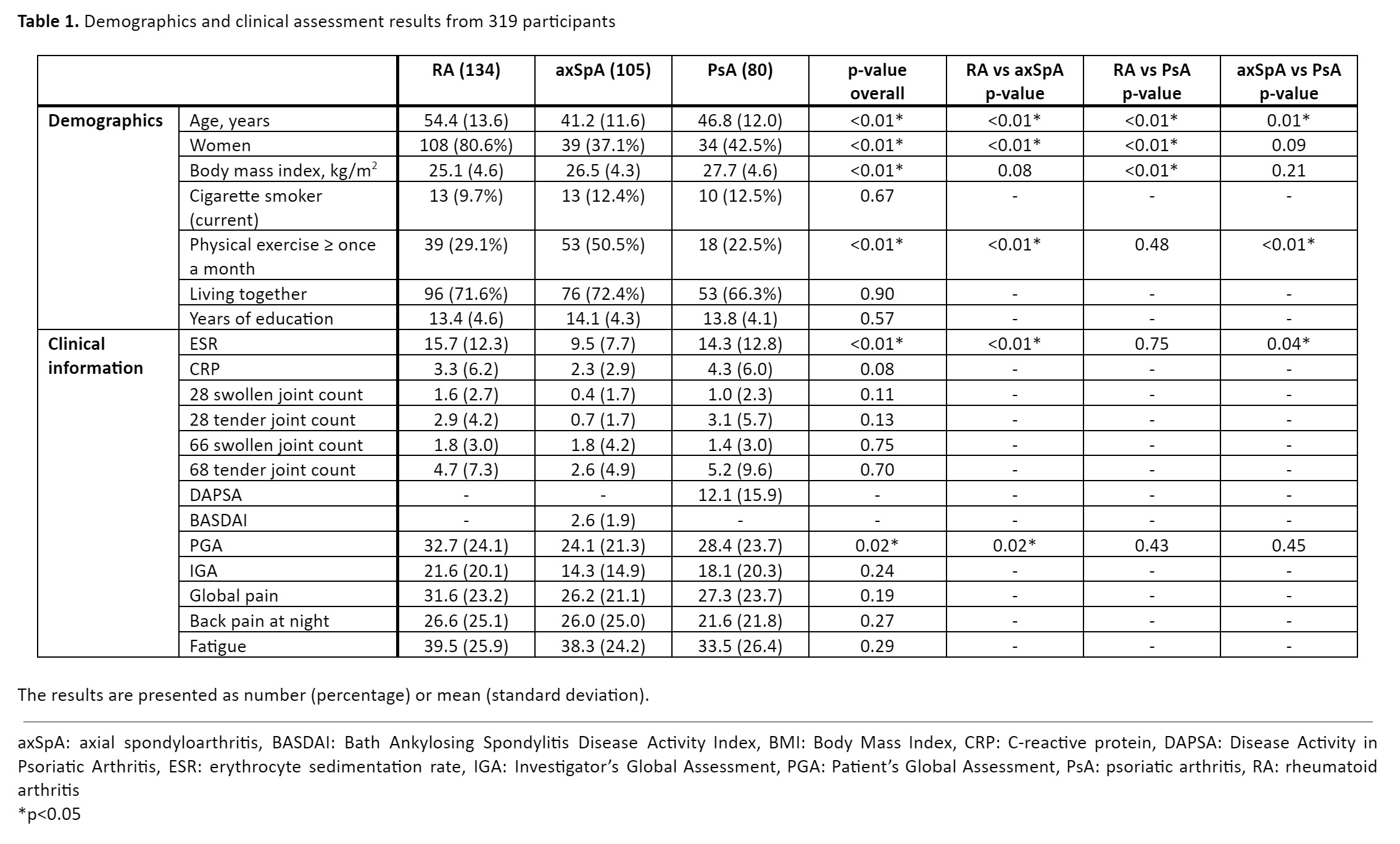
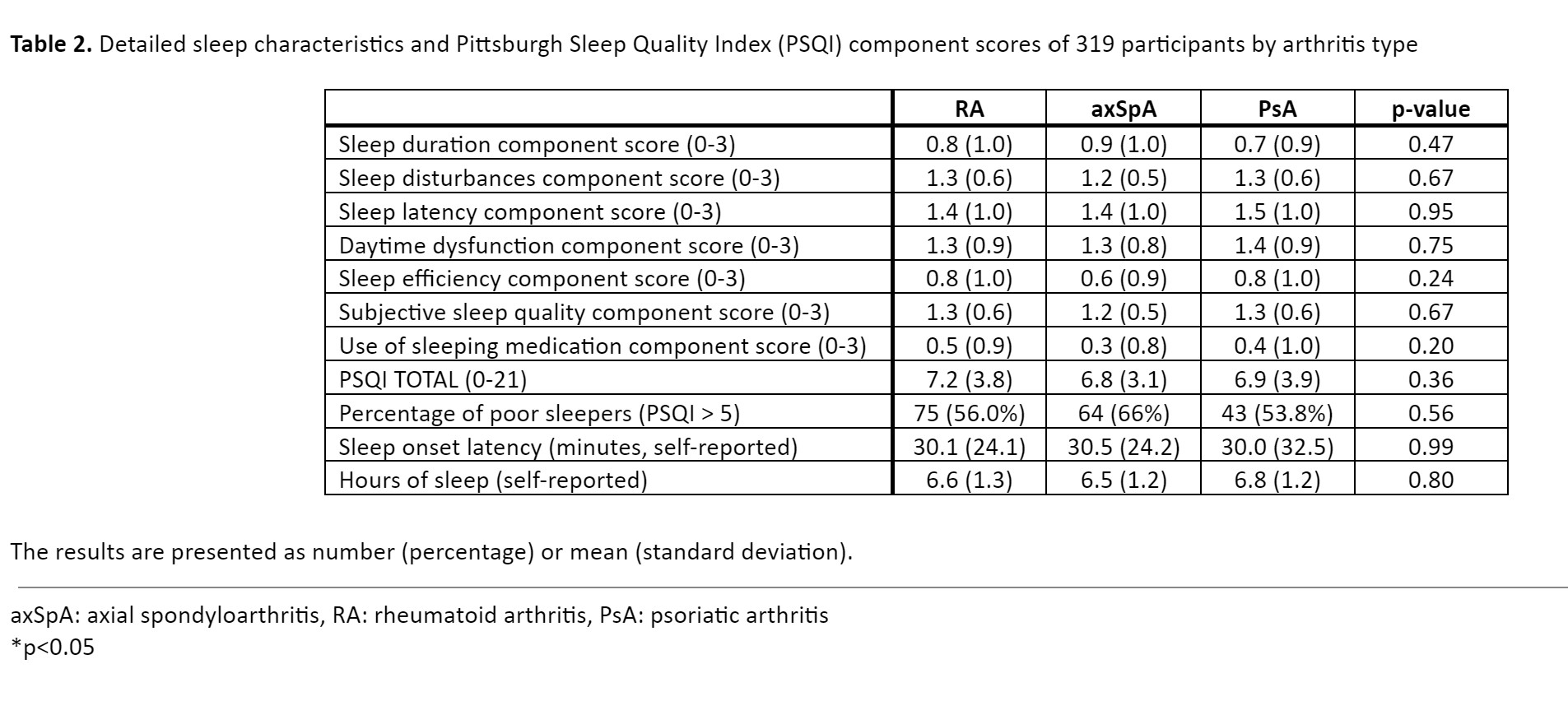
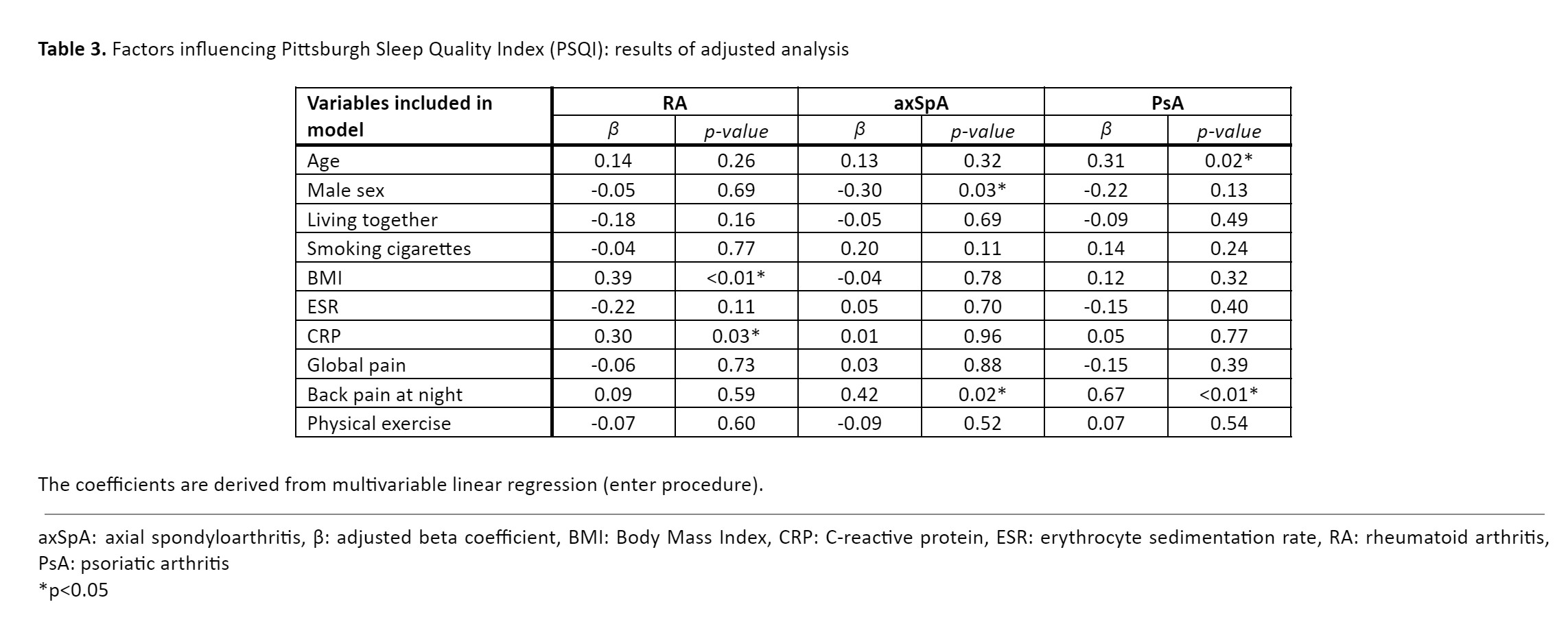
Methods: Cross sectional study of real-world data of 319 adult IA patients from PolNorRHEUMA registry utilizing GoTreatIT software. Variables obtained during routine outpatient visits included demographics, ESR, CRP, swollen and tender joint count, global pain, back pain at night, fatigue and disease activity scores: DAS28-CRP for RA, BASDAI for axSpA and DAPSA for PsA. Sleep quality was assessed using Pittsburgh Sleep Quality Index (PSQI) and scores higher than 5 were identified as poor sleep. All patients completed the Multidimensional Health Assessment Questionnaire (MDHAQ). Statistics included ANOVA with post-hoc (Tukey), Chi-square, and multivariable adjusted linear regression (enter procedure).
Results: We included 134 RA, 105 axSpA and 80 PsA patients. Patient characteristic is shown in Table 1. Prevalence of poor sleep varied from 53,8% in PsA, 56% in RA, to 66% in axSpA. No significant differences in consecutive sleep domains were identified (Table 2). However, we found slightly different independent risk factors for poor sleep as measured in PSQI (Table 3), namely higher BMI and increased level of CRP in RA and back pain at night in axSpA and PsA. Additional factors included female gender in axSpA and older age in PsA. In the baseline linear regression model, other variables such as SJC28, TJC28, and specific HAQ components (anxiety, depression, fatigue) were initially included as covariates. However, due to significant multicollinearity, we decided to remove them from the final model used in the analysis. We also found good correlation coefficients between the specific HAQ component related to sleep quality and PSQI score: 0.59 for RA (p< 0.01), 0.57 for axSpA (p< 0.01), and 0.65 for PsA (p< 0.01).
Conclusion: Our research confirms high prevalence of sleep disturbances in RA, axSpA and PsA, without differences in particular sleep domains but different independent risk factors for poor sleep. The HAQ component related to sleep quality could serve as a potential screening tool for identifying patients who may benefit from further sleep quality evaluation.
Disclosures: D. Polak: None; M. Wilk: None; P. Kuszmiersz: None; G. Haugeberg: None; M. Korkosz: None; Z. Guła: None.
To cite this abstract in AMA style:
Polak D, Wilk M, Kuszmiersz P, Haugeberg G, Korkosz M, Guła Z. Direct Comparison of Sleep Quality and Risk Factors for Poor Sleep Across Rheumatoid Arthritis, Axial Spondyloarthritis and Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/direct-comparison-of-sleep-quality-and-risk-factors-for-poor-sleep-across-rheumatoid-arthritis-axial-spondyloarthritis-and-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/direct-comparison-of-sleep-quality-and-risk-factors-for-poor-sleep-across-rheumatoid-arthritis-axial-spondyloarthritis-and-psoriatic-arthritis/