Session Information
Date: Saturday, November 12, 2022
Title: Health Services Research Poster I: Lupus, RA, Spondyloarthritis and More
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Disparities in long-term kidney outcomes have been documented in patients with childhood-onset systemic lupus erythematosus (cSLE) complicated by lupus nephritis (LN). However, there remains limited understanding of the impact of health care quality, including access to care, on disease outcomes. Our objective was to evaluate early care utilization patterns as a measure of access in individuals identified with cSLE and LN using a large, real-world database.
Methods: We utilized administrative claims data from IBM MarketScan Commercial and 8-State Medicaid Databases from 2006-2020. We identified individuals with cSLE using: 1) ≥3 ambulatory or inpatient claims with ICD-9 710.0 or ICD-10-CM M32.* (excluding M32.0) with ≥30 days between each code; 2) provider type pediatric rheumatology, rheumatology, pediatric nephrology, nephrology, dermatology, or acute care hospital; and 3) age ≥5 and < 18 years at the time of the first SLE code. We then selected patients with: 1) ≥182 days between insurance enrollment and the first SLE code; and 2) no evidence of anti-malarial or immunosuppressant use >182 days prior to the first SLE code to define incident cases. Finally, we identified cSLE patients with LN by ≥2 ambulatory or inpatient claims with ICD-9 580.*-586.*, 791.0 or ICD-10-CM M32.14, M32.15 with ≥30 days between. We abstracted sex, age at first SLE code, codes for dialysis, codes for kidney transplant, and time between first SLE and first LN code. For patients enrolled in commercial insurance, we abstracted US geographic region and population density. For those enrolled in Medicaid, we abstracted race and ethnicity. We divided patients by whether SLE codes or LN codes were used first. Descriptive statistics and bivariate analyses were conducted with significance levels set to 0.05.
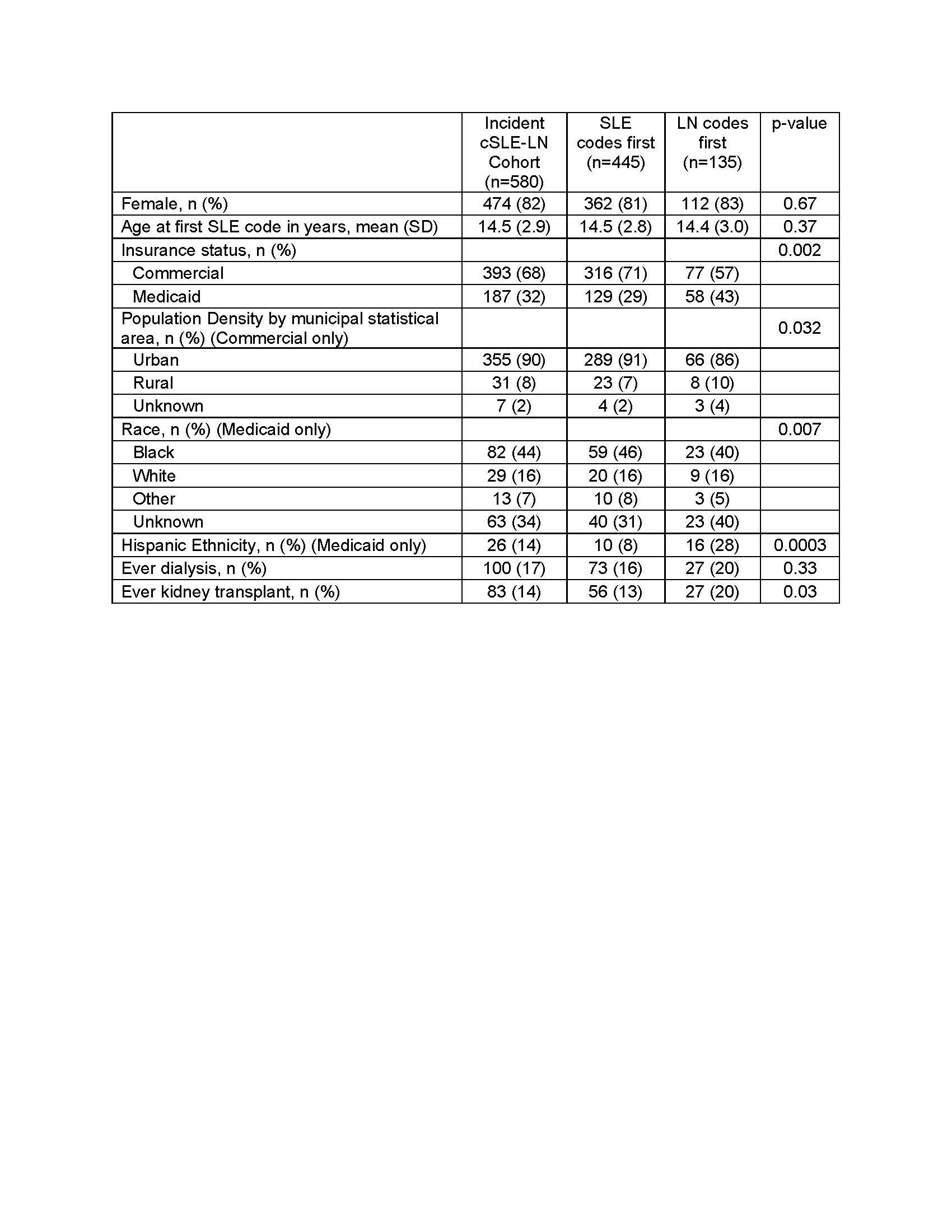
Results: We identified 580 individuals who met criteria for incident cSLE with LN. Patients with LN were 82% female and had a mean (SD) age at first SLE code of 14.5 (2.9) years (Table 1). In patients with commercial insurance, the majority were from the US South (51%), followed by West (18%), Northeast (16%), and Midwest (15%). We noted that while there was a mean (SD) time between first SLE and LN diagnosis codes of 0.5 (1.5) years, there was a range from -9.5 to 9.7 years. We grouped patients into those who received SLE codes first (77%) or LN codes first (23%). In the LN codes first group, we noted a statistically higher proportion of patients with Medicaid (43% vs 29%, p=0.002), living in a rural metropolitan statistical area (14% vs 9%, p=0.032), and of Hispanic ethnicity (28% vs 8%, p< 0.001). Patients with LN codes first were also more likely to have evidence of kidney transplant (20% vs 13%, p=0.03).
Conclusion: In this group of individuals identified with cSLE and LN, we noted two distinct patterns of whether patients first received SLE diagnosis codes or LN diagnosis codes. Patients who received LN codes before SLE codes were more likely to be publicly insured, live in a rural area, have Hispanic ethnicity, and have evidence of kidney transplant. Additional analyses are planned to better understand if these patterns reflect heterogeneous disease course or differential access to subspecialty care.
To cite this abstract in AMA style:
Smitherman E, Chahine R, Hersh A, Curtis J. Differential Diagnostic Coding Patterns and Associated Sociodemographic Factors in Childhood-Onset Lupus Nephritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/differential-diagnostic-coding-patterns-and-associated-sociodemographic-factors-in-childhood-onset-lupus-nephritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differential-diagnostic-coding-patterns-and-associated-sociodemographic-factors-in-childhood-onset-lupus-nephritis/