Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Dry Eye Disease (DED) is a common multifactorial condition that significantly impacts patient quality of life. The etiology of DED is complex, involving tear film instability, hyperosmolarity, ocular surface inflammation, and neuro-sensory abnormalities. Although Sjogren’s is a well-recognized cause of DED, the burden of Sjogren’s-related dry eye and its distinction from DED due to other etiologies remain poorly understood, with delayed diagnosis often leading to compounded morbidity. Our objective was to compare the severity of dry eye symptoms, systemic symptoms, and ocular surface and tear film parameters among these groups.
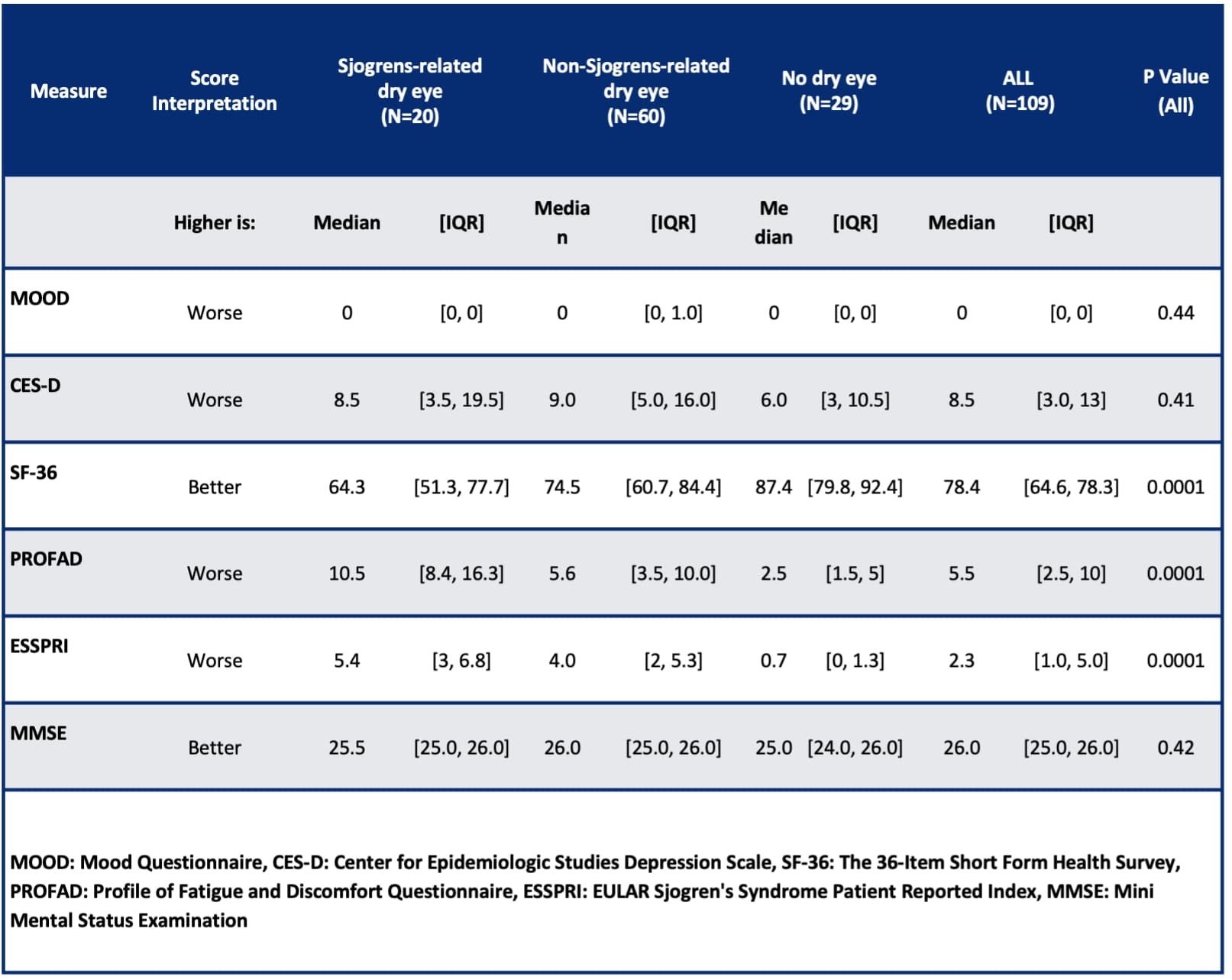
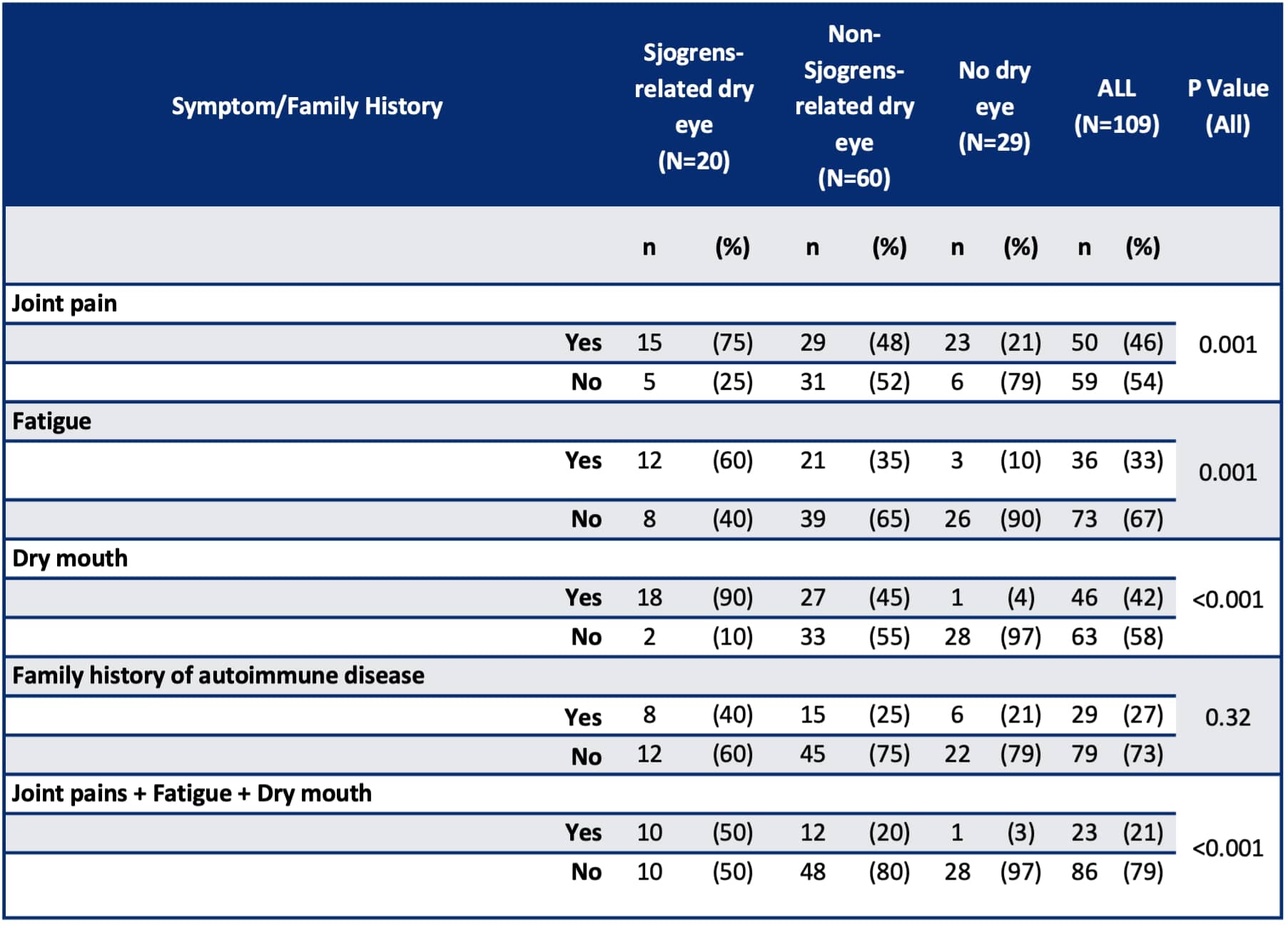
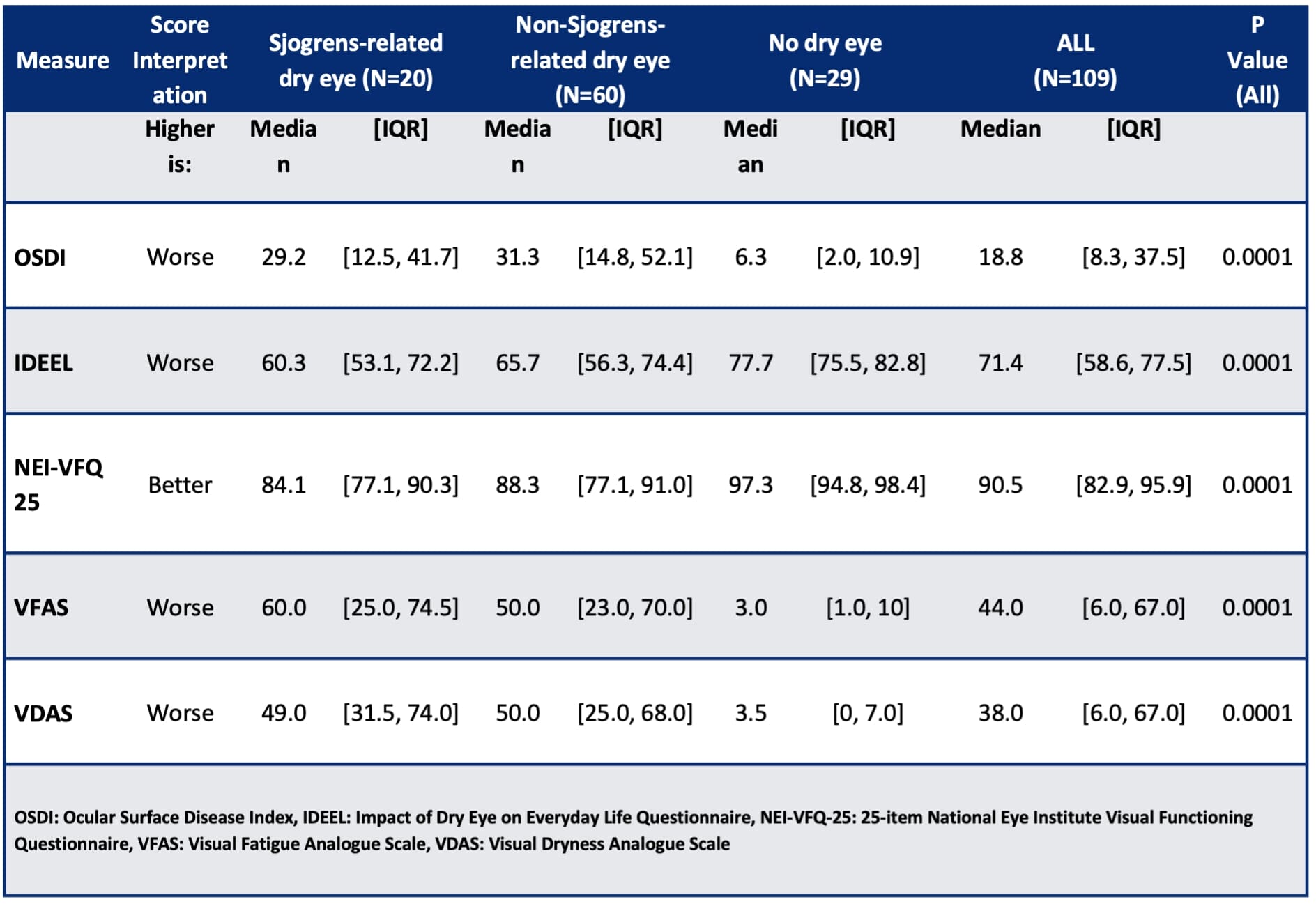
Methods: This case-control study included 109 participants across three groups: Sjogren’s-related dry eye (n=20), non-Sjogren’s dry eye (n=60), and a control group without dry eye (n=29). Participants were recruited from the Ocular Surface Diseases and Dry Eye Clinic at the Johns Hopkins Wilmer Eye Institute. Ocular and Sjogren’s-related symptoms were measured using the Ocular Surface Disease Index (OSDI) and the EULAR Sjogren’s Syndrome Patient Reported Index (ESSPRI), respectively. Quality of life was measured using the SF-36 Health Survey. Statistical analysis was conducted using STATA/BE 18.0, with the Kruskal-Wallis and Chi-square tests applied for comparing continuous and categorical variables respectively.
Results: Participants with Sjogren’s-related dry eye experienced significantly worse quality of life and higher symptom severity than those with non-Sjogren’s dry eye and controls. Key findings include higher OSDI scores in the Sjogren’s group than the non-Sjogren’s dry eye group and controls: median 29.2 (interquartile range [IQR] 12.5-41.7) versus 31.3 (IQR 14.8-52.1) versus 6.3 (IQR 2.0-10.9), respectively (P< 0.001). Systemic symptoms, such as joint pain and fatigue, were more prevalent in the Sjogren’s group, with 75% and 60% of patients reporting these issues, respectively, significantly higher than the other groups (P=0.001 for both). Median ESSPRI scores were considerably higher in the Sjogren’s group (5.4, IQR 3-6.8) than the non-Sjogren’s group (4, IQR 2-5.3) and controls (0.7, IQR 0-1.3) (P< 0.001). The Sjogren’s group had lower median SF-36 scores (64.3, IQR 51.3-77.7) than the non-Sjogren’s group (74.5, IQR 60.7-84.4) and controls (87.4, IQR 79.8-92.4) (P< 0.001).
Conclusion: The study underscores the substantial impact of Sjogren’s on individuals with dry eye, highlighting the need for early diagnosis and targeted management strategies. It also emphasizes the importance of distinguishing between Sjogren’s-related dry eye and non-Sjogren’s dry eye. We suggest a multidisciplinary treatment framework integrating both ophthalmological and rheumatological care to enhance patient outcomes.
To cite this abstract in AMA style:
Akpek E, Saldanha I, Bareamichael P, Lin M. Differential Diagnosis of Sjogren’s vs Non-Sjogren’s Dry Eye [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/differential-diagnosis-of-sjogrens-vs-non-sjogrens-dry-eye/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differential-diagnosis-of-sjogrens-vs-non-sjogrens-dry-eye/