Session Information
Date: Monday, November 13, 2023
Title: (1221–1255) Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Juvenile dermatomyositis (JDM) is characterized by multiorgan vasculopathy, and degree of vasculopathy can indicate more severe disease. Nailfold capillaroscopy is a non-invasive method to directly evaluate abnormalities in the microvasculature. While the majority of children with JDM present with nailfold capillary (NFC) abnormalities, we do not fully understand whether NFC patterns and characteristics might differentiate JDM from other pediatric autoimmune diseases or lend insight into distinct JDM subgroups. In this study, we utilized high-resolution nailfold video capillaroscopy paired with a machine learning approach to (1) generate patient subgroups based on NFC features and (2) characterize clinical features defining each patient subgroup.
Methods: We utilized nailfold video capillaroscopy at 200x to obtain images from JDM (n=23), childhood systemic lupus erythematosus (SLE) (n=9), mixed connective tissue disease (MCTD) (n=5) and healthy control (n=17) patients at the University of Michigan Pediatric Rheumatology Clinic (1/1/23 – 5/31/23). We quantified NFC features from images using a convolutional neural network via an automated method, including density of normal and giant capillaries, microhemorrhages, and percentage of enlarged, tortuous or ramified capillaries. We then performed unsupervised cluster analysis to identify patients with similar NFC features. Following this, clinical variables were grouped by cluster with differences between means assessed for significance by ANOVA (p≤0.05).
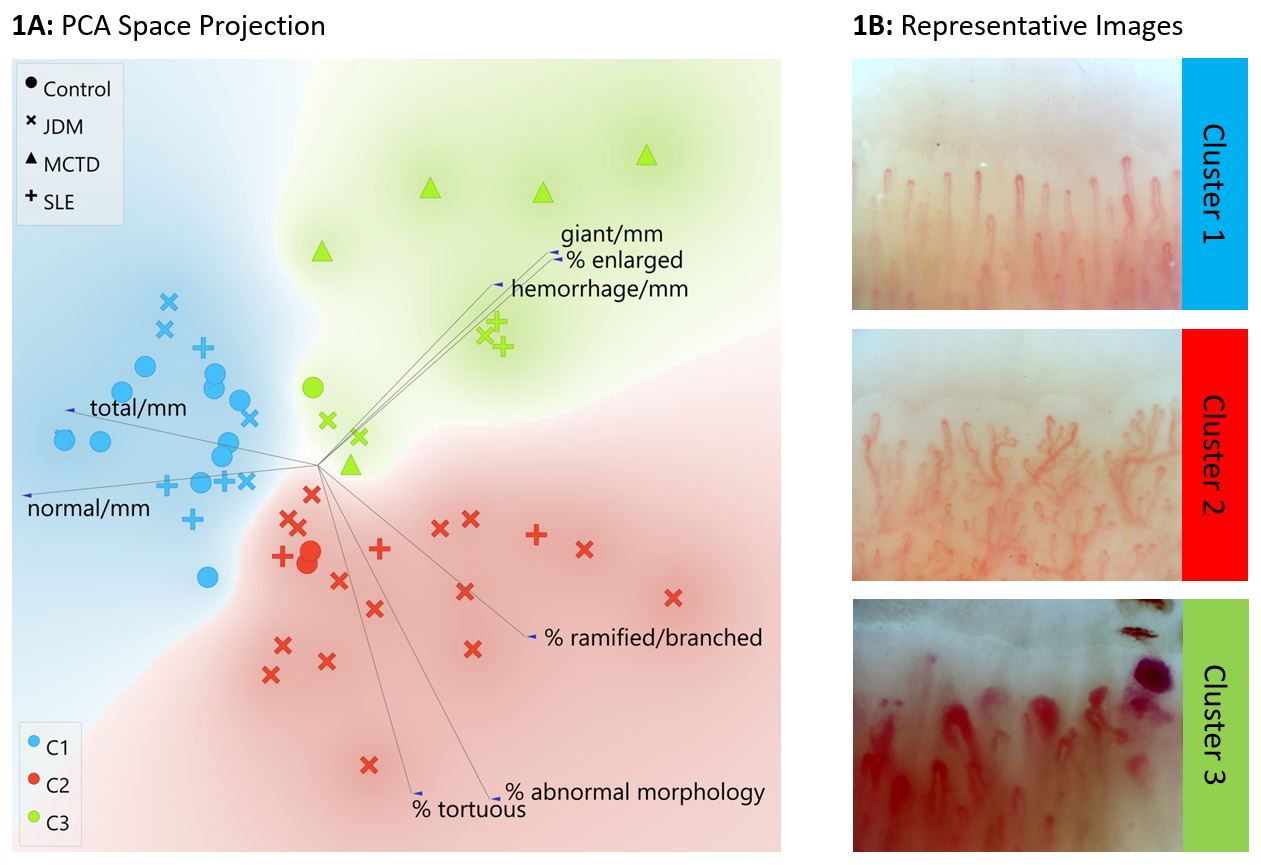
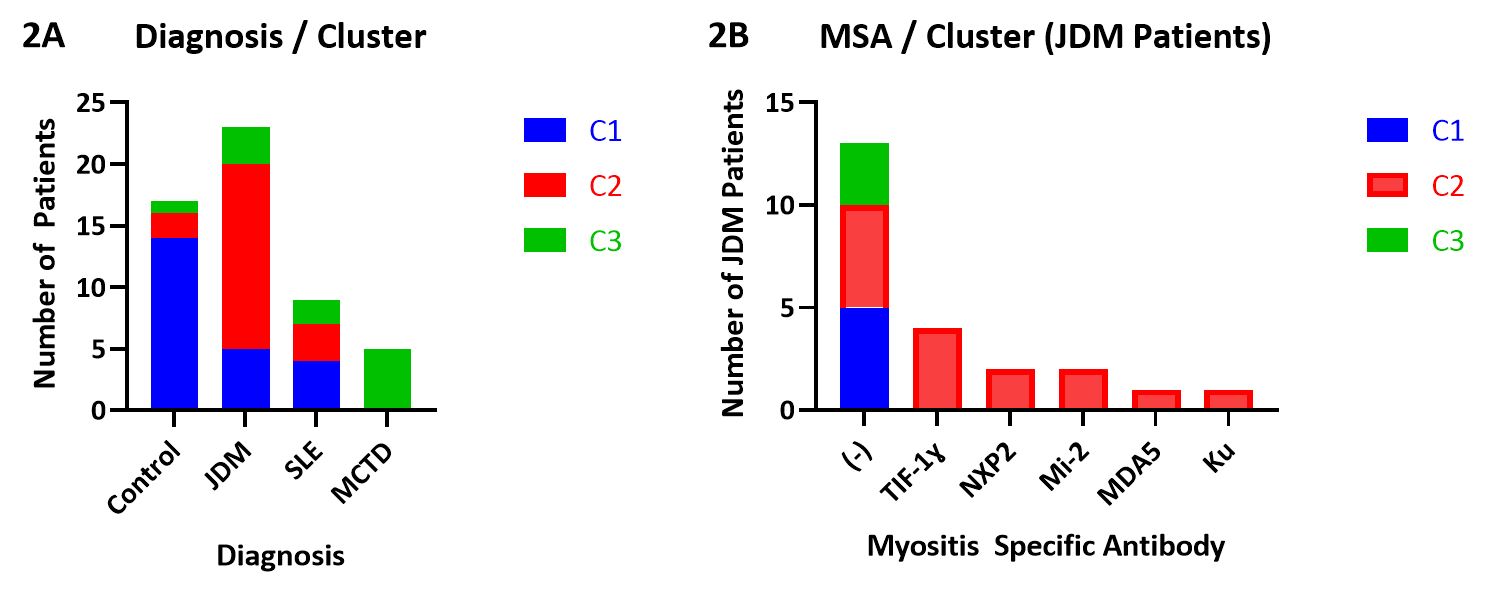
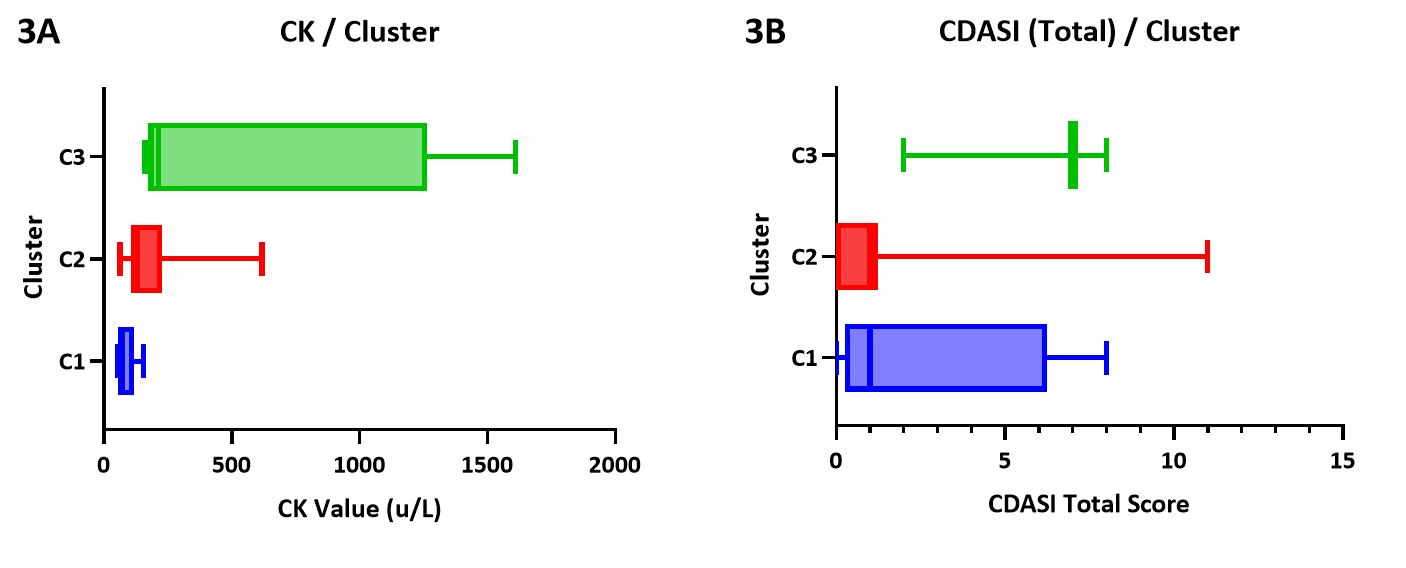
Results: We identified 3 patient clusters distinguished by a predominant NFC pattern of either higher relative capillary density (cluster 1 (C1)), abnormal morphology (C2) or enlarged capillaries (C3) (Figure 1). Upon review of JDM clinical features by cluster, we found JDM patients were primarily assigned to C2 (65%), with the remainder in C1 (22%) and C3 (13%). MCTD patients were entirely assigned to C3 (100%). Patients with SLE were distributed more evenly, with 44%, 33%, and 22% in C1, 2, and 3, respectively. The majority of control patients were assigned to C1 (82%) (Figure 2A). Interestingly, we found that all JDM patients with presence of a positive MSA (TIF-1γ, MDA5, NXP2, Mi-2, Ku) were assigned to C2, while those with negative MSAs were spread between C1, 2 and 3 (Figure 2B). We assessed CK values by cluster, revealing a trend toward higher CK in C3 (mean 550.8 u/L) than C2 (mean 201.2 u/L) or C1 (mean 83.6) (Figure 3A, p=0.073). Aldolase and LDH levels were similar between clusters (p=0.65 and p=0.77, respectively). Skin disease activity as assessed by Cutaneous Dermatomyositis Disease Area and Severity Index (CDASI) scores trended toward higher values in C3 (mean 5.7) as compared to C2 (mean 1.5) and C1 (mean 2.5) (Figure 3B, p=0.124).
Conclusion: We demonstrate 3 distinct groupings of NFC patterns that align with clinical diagnosis and MSA positivity. A predominant pattern of tortuosity and ramification is most pronounced in JDM as compared to MCTD, SLE and control patients. Further investigation into NFC morphology and patterns within a larger JDM cohort may hold the potential to assist in diagnosis, disease subtyping, monitoring and prognostication.
To cite this abstract in AMA style:
McClellan N, Vandenbergen S, Matossian S, Kahlenberg J, Turnier J. Differences in Nailfold Capillary Morphology Distinguish Juvenile Dermatomyositis Patients That Are Myositis-Specific Autoantibody Positive [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/differences-in-nailfold-capillary-morphology-distinguish-juvenile-dermatomyositis-patients-that-are-myositis-specific-autoantibody-positive/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differences-in-nailfold-capillary-morphology-distinguish-juvenile-dermatomyositis-patients-that-are-myositis-specific-autoantibody-positive/