Session Information
Date: Sunday, November 13, 2016
Title: Systemic Lupus Erythematosus – Clinical Aspects and Treatment II: Clinical Trial Design
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: The CLSP is a population-based registry of individuals with SLE residing in San Francisco County, California from 2007 – 2009. The registry has a special focus on improving our understanding of SLE in Asian/Pacific Islander (PI) and Hispanic individuals, two groups previously understudied in population-based epidemiologic investigations. We used CLSP data to analyze differences in 1) lupus manifestations by sex and race/ethnicity and 2) time to development of these manifestations after disease onset.
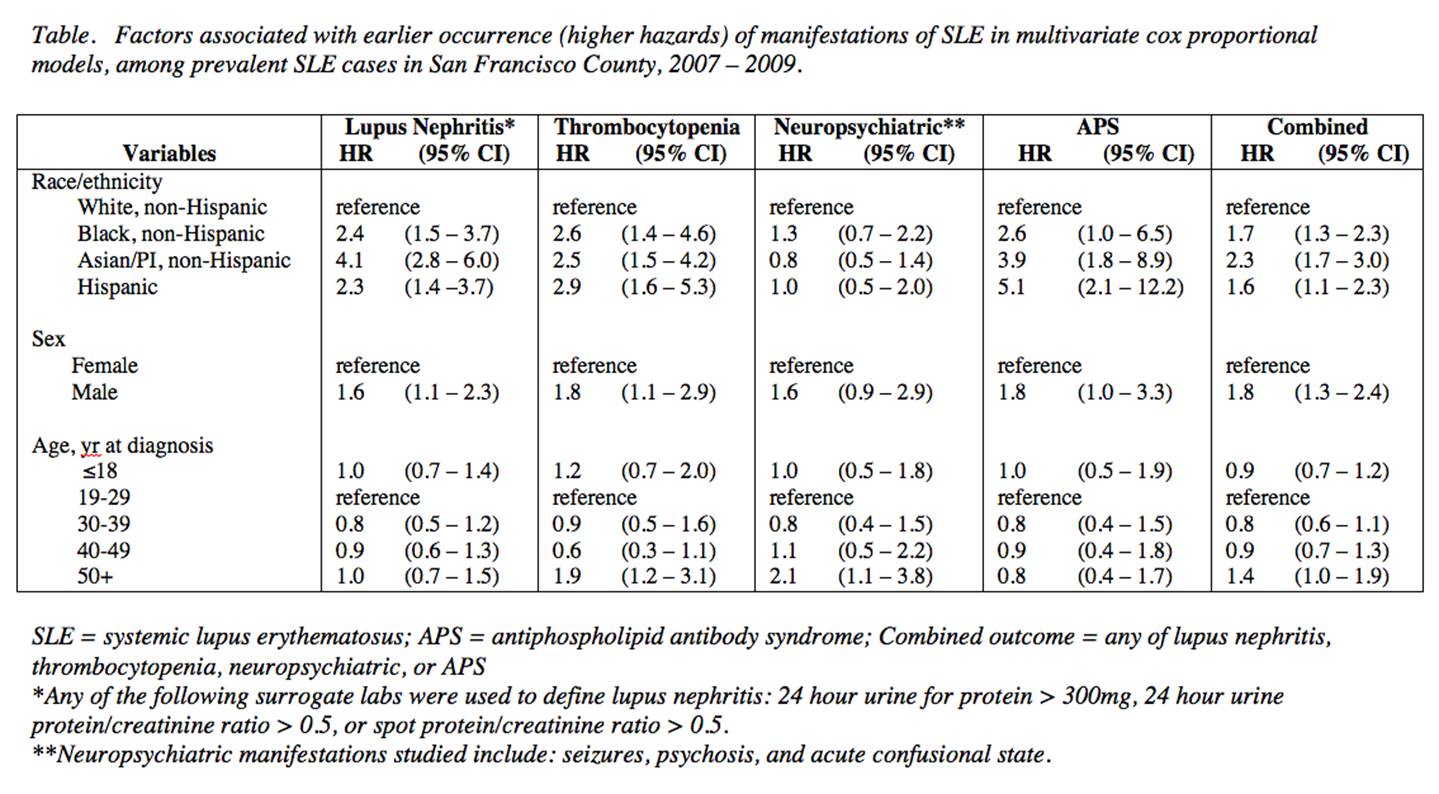
Methods: Relative risks (RR) of SLE manifestations were calculated using Poisson regression models adjusted for race/ethnicity, sex, age at SLE diagnosis, and duration of SLE disease. Kaplan-Meier and Cox proportional hazards methods were used to analyze time to development of severe manifestations of SLE, with higher hazard ratios (HR) indicating a shorter time to development of specific manifestations.
Results: 724 prevalent cases of SLE were identified with the following distribution by race/ethnicity: white (26.2%), Black (18.8%), Asian/PI (36.9%), Hispanic (15.5%), missing (2.6%). For lupus manifestations, Blacks, Asians/PIs, and Hispanics had increased prevalence of lupus nephritis relative to whites (RR 1.78, RR 1.74, and RR 1.46, respectively). Furthermore, Blacks had increased neurological manifestations (RR 1.50), Asians/PIs had increased mucocutaneous manifestations (RR 1.16), and both Blacks and Asians/PIs had increased hematologic manifestations (RR 1.08 and RR 1.07, respectively). For time to development of manifestations, statistically significant differences in lupus nephritis (p < 0.001), thrombocytopenia (p = 0.006), and neuropsychiatric abnormalities (p = 0.042) were observed by race/ethnicity, though this was not the case in the analysis of antiphospholipid (APS) (P = 0.092). Blacks, Asians/PIs, and Hispanics had earlier development (higher hazards) of lupus nephritis, thrombocytopenia, and APS relative to whites. Men had earlier development of lupus nephritis and thrombocytopenia relative to women (Table).
Conclusion: This analysis represents the first epidemiologic study comparing lupus manifestations among four major racial/ethnic groups and includes large numbers of Asians/PIs and Hispanics. We found 1) dramatic differences in the prevalence of several clinical SLE manifestations among race/ethnicities and 2) that Blacks, Asians/PIs, and Hispanics are at increased risk of developing many manifestations earlier than whites following initial SLE diagnosis. Men also developed lupus nephritis and thrombocytopenia earlier than women with SLE.
To cite this abstract in AMA style:
Maningding E, Yazdany J, Trupin L, Tonner C, Helmick CG, Dall'Era M. Differences in Clinical Manifestations of SLE Across Four Racial/Ethnic Groups: The California Lupus Surveillance Project (CLSP) [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/differences-in-clinical-manifestations-of-sle-across-four-racialethnic-groups-the-california-lupus-surveillance-project-clsp/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differences-in-clinical-manifestations-of-sle-across-four-racialethnic-groups-the-california-lupus-surveillance-project-clsp/