Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Major salivary glands ultrasound (SGU) is a promising tool in the diagnosis of Sjögren syndrome (SS) and has demonstrated good sensitivity and specificity in previous studies. However, its usefulness in daily rheumatology practice has not been completely established.
The objective of this study was to assess the performance of SGU for diagnose of SS in routine clinical practice.
Methods: This was a cross-sectional single center observational study. Patients with clinical suspicion (due to xerostomia, xerophthalmia or positive anti-Ro) or confirmed diagnosis of SS were included in the study. All patients underwent sialometry, Schirmer test and blood samples, including autoantibodies, as part of the routine clinical practice. SGU was performed in all patients by a rheumatologist who was unaware of clinical data. OMERACT semi-quantitative scoring system for SGU that grades each gland from 0 to 3 (parotid and submandibular) was evaluated. A cutoff of ≥2 in any of the four glands was selected because has shown good performance for the diagnosis of SS in previous studies. Demographic data and clinical history were collected, including minor salivary gland biopsy when available. Fulfilment of 2016 ACR/EULAR criteria for SS [2] was evaluated in each patient. Sensitivity, specificity, positive predictive value, and negative predictive value were calculated for sialometry and SGU.
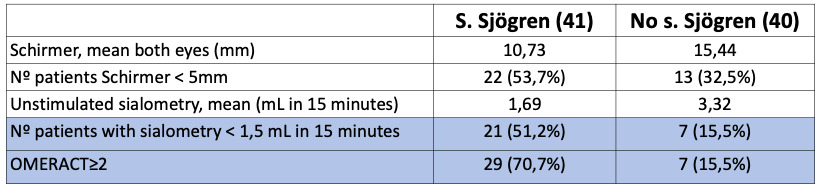
Results: 81 patients were included, of which 76 (93.8%) were women. Of the total, 41 (50.6%) met the 2016 ACR/EULAR SS criteria. Anti-Ro/SSA antibody was positive in 54/81 (66.7%) and minor salivary gland biopsy was performed in 8 (9.9%) patients, being pathological in 6 (7.4%). Of the 40 patients who did not meet criteria for classification as SS, 13 (32.5%) had a Schirmer test < 5 mm, 7 (15.5%) had a basal sialometry < 1.5 mL in 15 minutes and 7 (17.5%) had an SGU with OMERACT ≥2. Of the 41 patients classified as SS, 22 (53.7%) had pathological Schirmer, 21 (51.2%) had a basal sialometry < 1.5 mL in 15 minutes and 29 (70.7%) had an SGU with OMERACT ≥ 2.
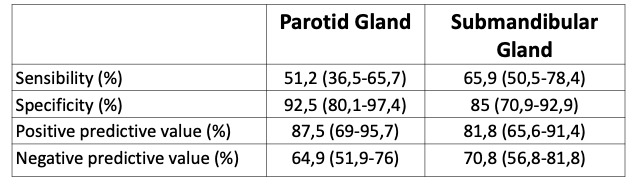
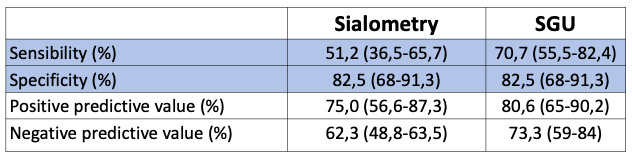
Sialometry had a sensitivity of 51.2% (36.5-65.7%) and a specificity of 82.5% (68.0-91.3%) for classification as SS, and SGU (OMERACT ≥2) had a sensitivity of 70.7% (55.5-82.4%) and a specificity of 82.5% (68.0-91.3%). The positive predictive value of the SGU was 80.6% (65.0-90.2%) and the negative predictive value was 73.3% (59.0-84.0%).
Conclusion: In our routine clinical practice, the diagnostic performance of SGU is good, superior to sialometry, although the latter is included in the ACR/EULAR criteria for SS and the SGU not.
To cite this abstract in AMA style:
Raya-Santos C, Senabre J, Bernal J, Gallego Campuzano R, Pons-Canet L, Pons-Bas A, Cortes J, Santos-Soler G, Rosas-Gómez de Salazar J. Diagnostic Performance of Mayor Salivary Gland Ultrasound for Diagnosis of Sjögren’s Syndrome in Routine Clinical Practice [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/diagnostic-performance-of-mayor-salivary-gland-ultrasound-for-diagnosis-of-sjogrens-syndrome-in-routine-clinical-practice/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diagnostic-performance-of-mayor-salivary-gland-ultrasound-for-diagnosis-of-sjogrens-syndrome-in-routine-clinical-practice/