Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
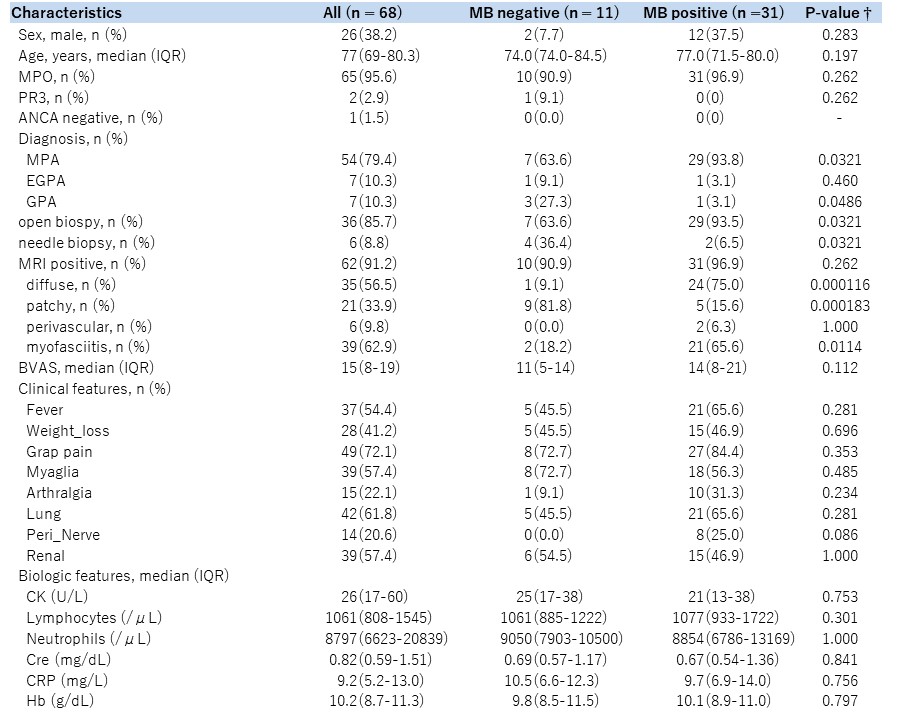
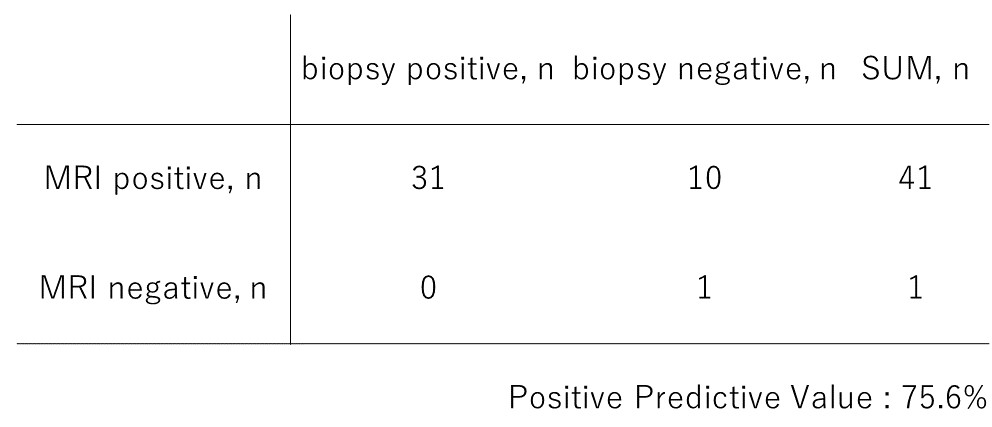
Background/Purpose: Histopathologic confirmation is the golden standard for diagnosis of anti-neutrophil cytoplasmic antibody-associated vasculitis (AAV), but sometimes can be difficult because of its invasion (e.g. renal biopsy) or low diagnostic yield (e.g. otorhinolaryngological biopsy). Some studies suggest that muscle biopsy (MB) is a useful tool for diagnosis of AAV owing to its safety and high diagnostic yield and muscle MRI could guide the site of MB [1]. However, there are no previous studies focusing on diagnostic yield of muscle MRI for systemic vasculitis. We aimed to assess the positive predictive value (PPV) of a muscle MRI for MB and describe the muscle MRI features of systemic vasculitis.
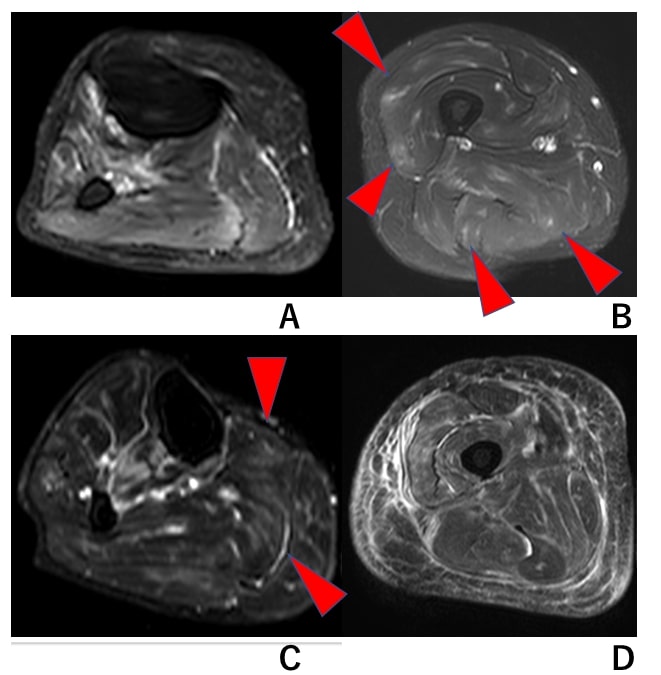
Methods: We included all AAV patients who performed muscle MRI at diagnosis or recurrence in our center between 2009 and 2020. The proof of muscular vasculitis was based on the presence of necrotizing vasculitis on MB. As previously reported in polyarteritis nodosa, MRI findings are evaluated with a focus on muscle and fascial lesions. Muscle MRI findings were classified into the following four categories: “diffuse”, “patchy”, “perivascular”, and “myofasciitis” [2]. Duplication of MRI findings was allowed and counted in each category. We calculated PPV of muscle MRI for muscular vasculitis and compared characteristics of the patients with MB positive and those with MB negative.
Results: Among 68 AAV patients with a muscle MRI performed, 62 patients had a positive finding of muscle MRI. Of the positive MRI results, 35 patients (56.5%) presented diffuse pattern, 21 (33.9%) patients presented patchy pattern, and 6 patients (9.8%) presented perivascular pattern, and 39 patients (62.9%) had myofasciitis pattern. Among 39 patients with myofasciitis, there were 29 patients with diffuse pattern, 8 with patchy pattern, 2 with perivascular pattern, and none with myofasciitis alone. Open biopsy was performed in 36 patients (85.7%), and needle biopsy was performed in 6 patients. 31 patients were positive for MB, 10 patients were negative for MB. Among the patients underwent MB, PPV of a muscle MRI for muscular vasculitis was 75.6% (31/41). Comparing MB positive patients and MB negative patients, the clinical diagnosis of MPA (93.8% vs 63.6%), receiving open biopsy (93.5% vs 63.9%), and the diffuse pattern (75.0% vs 9.1%) and myofasciitis pattern (65.6% vs 18.2%) were significantly higher in MB positive patients. There was no significant difference in clinical and laboratory features including vascular disease activity between the two groups.
Conclusion: Muscle MRI can predict the positivity of MB and muscular vasculitis with a high probability. In addition, specific MRI findings (diffuse and myofasciitis patterns) can predict a positive muscle biopsy with high probability.
[1] Mathieu L et al. Muscle biopsy in anti-neutrophil cytoplasmic antibody-associated vasculitis: diagnostic yield depends on anti-neutrophil cytoplasmic antibody type, sex and neutrophil count. Rheumatology 2021; 60:699-707.
[2] Yusuhn K et al. Muscle involvement in polyarteritis nodosa: report of eight cases with characteristic contrast enhancement pattern on MRI. AJR2016; 206:378-384.
To cite this abstract in AMA style:
Inaba R, Waki D, Nishimura K, Yoshida T, Mizukawa K, Yamamoto S, Iri O, Yo K, Murabe H. Diagnostic Accuracy of Muscle MRI for Muscular Vasculitis in Anti-neutrophil Cytoplasmic Antibody-associated Vasculitis: A Pilot Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/diagnostic-accuracy-of-muscle-mri-for-muscular-vasculitis-in-anti-neutrophil-cytoplasmic-antibody-associated-vasculitis-a-pilot-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diagnostic-accuracy-of-muscle-mri-for-muscular-vasculitis-in-anti-neutrophil-cytoplasmic-antibody-associated-vasculitis-a-pilot-study/