Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: MRI is becoming the OA imaging modality of choice. It allows quantification of cartilage damage, the signature pathologic feature of disease. Proposed MRI-based definitions of OA have limitations, including inconsistency across tibiofemoral (TF) versus patellofemoral (PF) compartments and the possibility of satisfying the OA definition without cartilage damage despite this being a hallmark feature of OA. A definition should not consider cartilage damage as a sole criterion as it also occurs following joint trauma in the absence of OA; and should include osteophytes, which represent a bony response to cartilage loss. Using radiographic and symptomatic/radiographic OA as gold standards, we calculated the sensitivity and specificity of MRI-based definitions of knee OA that included cartilage damage and osteophytes as required criteria and tested whether inclusion of bone marrow lesions or synovitis, features associated with pain and disease progression, improved diagnostic performance.
Methods: Participants from the Multicenter Osteoarthritis (MOST) study, a longitudinal prospective cohort of older adults with knee x-rays and MRIs at the 30-month study visit, were included in this cross-sectional analysis. Whole knee radiographic OA (ROA) was defined as Kellgren-Lawrence (KL) grade ≥2 in either the TF or PF joint. Symptomatic ROA (SxROA) was defined as ROA with frequent knee pain in the affected knee. MRI abnormalities were scored using the WORMS scale in 14 regions in the TF and PF joints, including cartilage (scored 0-6 with definite cartilage damage scored ≥2), osteophytes (0-6), and either presence of bone marrow lesions (BMLs) (0-3), or effusion/synovitis or synovitis (0-3 at 3 sites). For each feature, we chose the worst WORMS score in the knee.
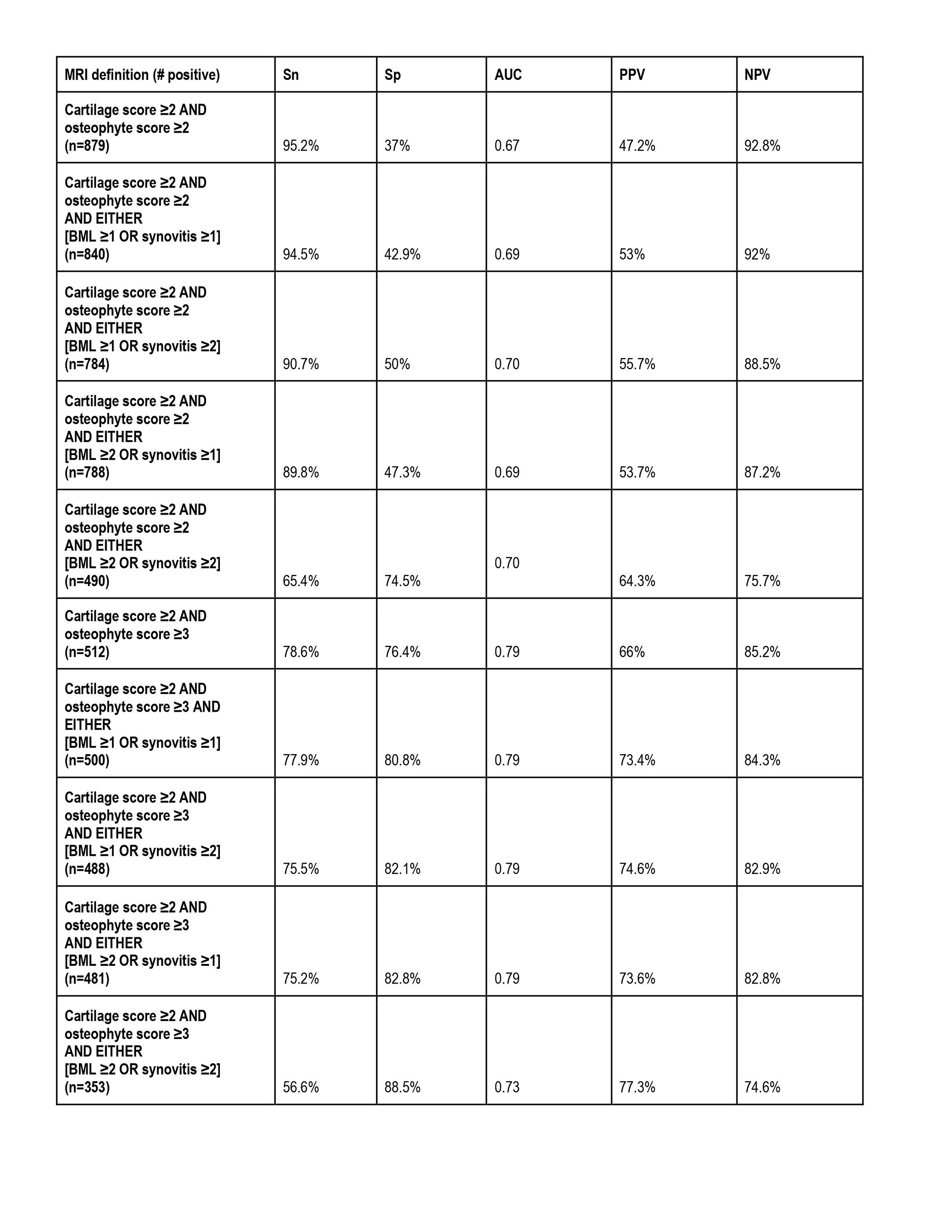
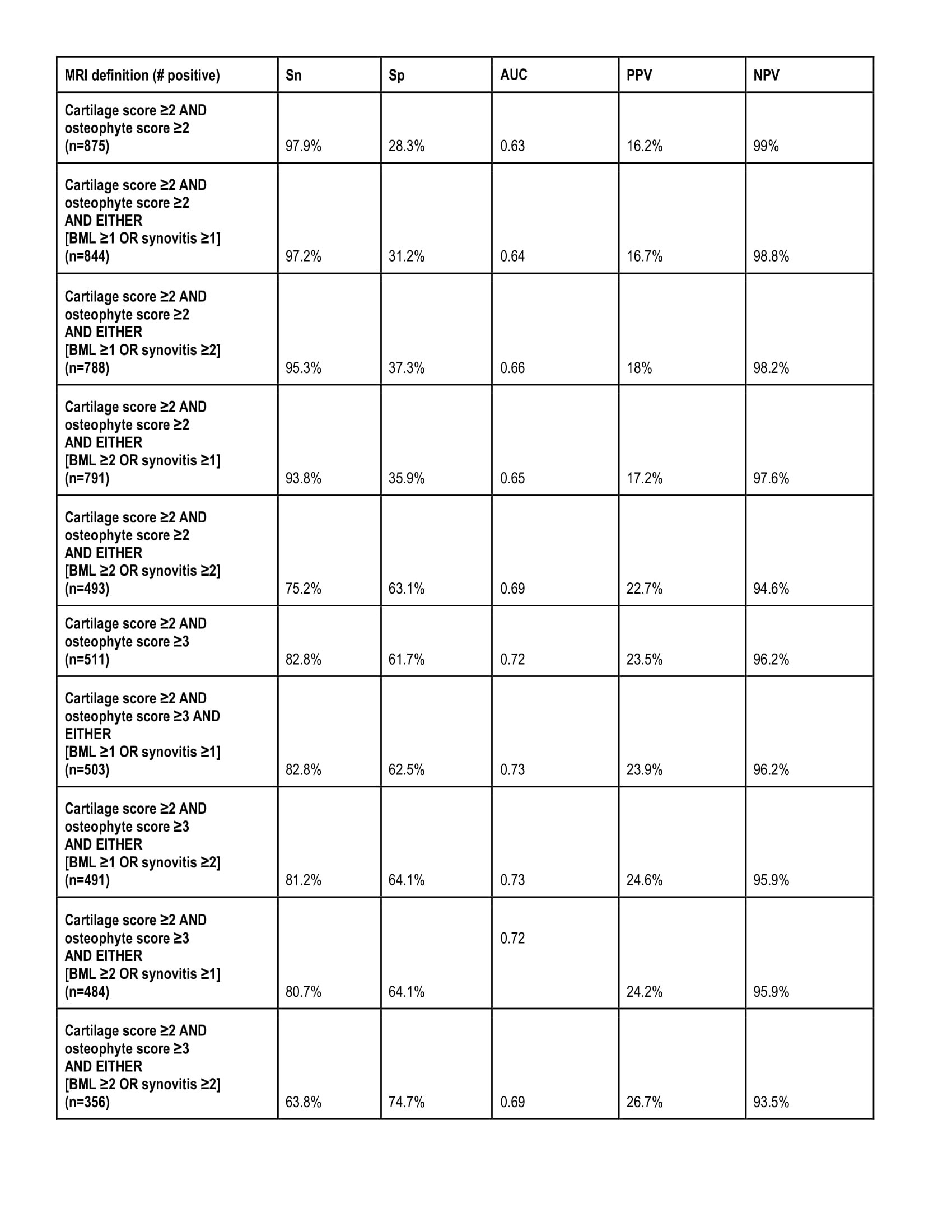
We tested different combinations of MRI features, which we compared to the gold standards of prevalent ROA and SxROA. Combinations of MRI features included cartilage damage (WORMS ≥2) and osteophyte score ≥2 (alternatively, ≥3). In addition, we tested definitions that included BMLs (score ≥1 or ≥2) and synovitis (≥1 or ≥2). For each MRI OA definition, we calculated sensitivity (Sn), specificity (Sp), positive and negative predictive values (PPV and NPV) and the area under the curve (AUC). We chose the definition with highest AUC that preserved Sn ≥ 80% for ROA.
Results: We included 1185 individuals (1185 knees) (mean age 61 years, 62% female, 89% white). Of these, 316 had prevalent ROA and 83 prevalent SxROA. The best performing definitions for both ROA and SxROA required not only cartilage damage and osteophytes but either mild-moderate BMLs or synovitis (Sn 90.7%, Sp 50%, AUC 0.70 for ROA).
Conclusion: We tested MRI-based definitions for OA, that all included cartilage damage and allowed for consistency across the TF and PF compartments, against the gold standards of prevalent ROA and SxROA. We found that a definition involving cartilage damage, osteophytes, and the presence of either moderate BMLs or synovitis had the best metrics for identifying ROA and SxROA. This improves on proposed definitions that could leave cartilage out and provided inconsistent disease definitions across compartments.
To cite this abstract in AMA style:
Liew J, Rabasa G, LaValley M, collins J, Stefanik J, Guermazi A, Lewis C, Nevitt M, Torner J, Felson D. Development of an MRI-based Definition of Knee Osteoarthritis: Data from the Multicenter Osteoarthritis Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/development-of-an-mri-based-definition-of-knee-osteoarthritis-data-from-the-multicenter-osteoarthritis-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/development-of-an-mri-based-definition-of-knee-osteoarthritis-data-from-the-multicenter-osteoarthritis-study/