Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Hyperuricemia is associated with an elevated risk of developing cardiovascular diseases, diabetes, chronic kidney disease, and metabolic syndromes. The Hmong population, in particular, has a higher predisposition to hyperuricemia/gout and other comorbid conditions associated. These diseases also occur at much younger ages in this population. More recently, studies have shown that all individuals with gout have higher risk of morbidity and mortality with COVID-19 infection. We examined outcomes of COVID-19 infection in the Hmong population with gout to determine whether these effects were magnified and of even greater import.
Methods: We conducted a retrospective cohort study on patients ≥ 18 years old with documented COVID-19 infection requiring oxygen who were admitted to two tertiary care centers between March 1, 2020- December 31, 2021. COVID-19 outcomes including ventilatory support, 30-day mortality, and length of stay were compared between Hmong and non-Hmong cohorts. This abstract presents a descriptive analysis of COVID-19 outcomes in the Hmong population with gout compared to COVID-19 outcomes in the Hmong population without gout and other non-Hmong cohorts.
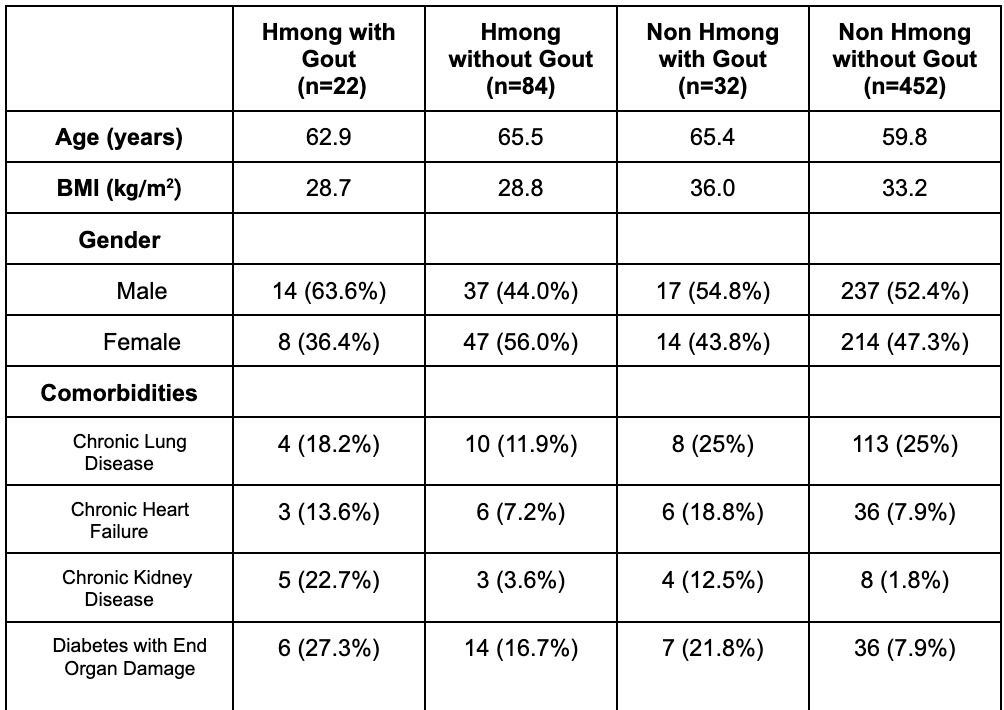
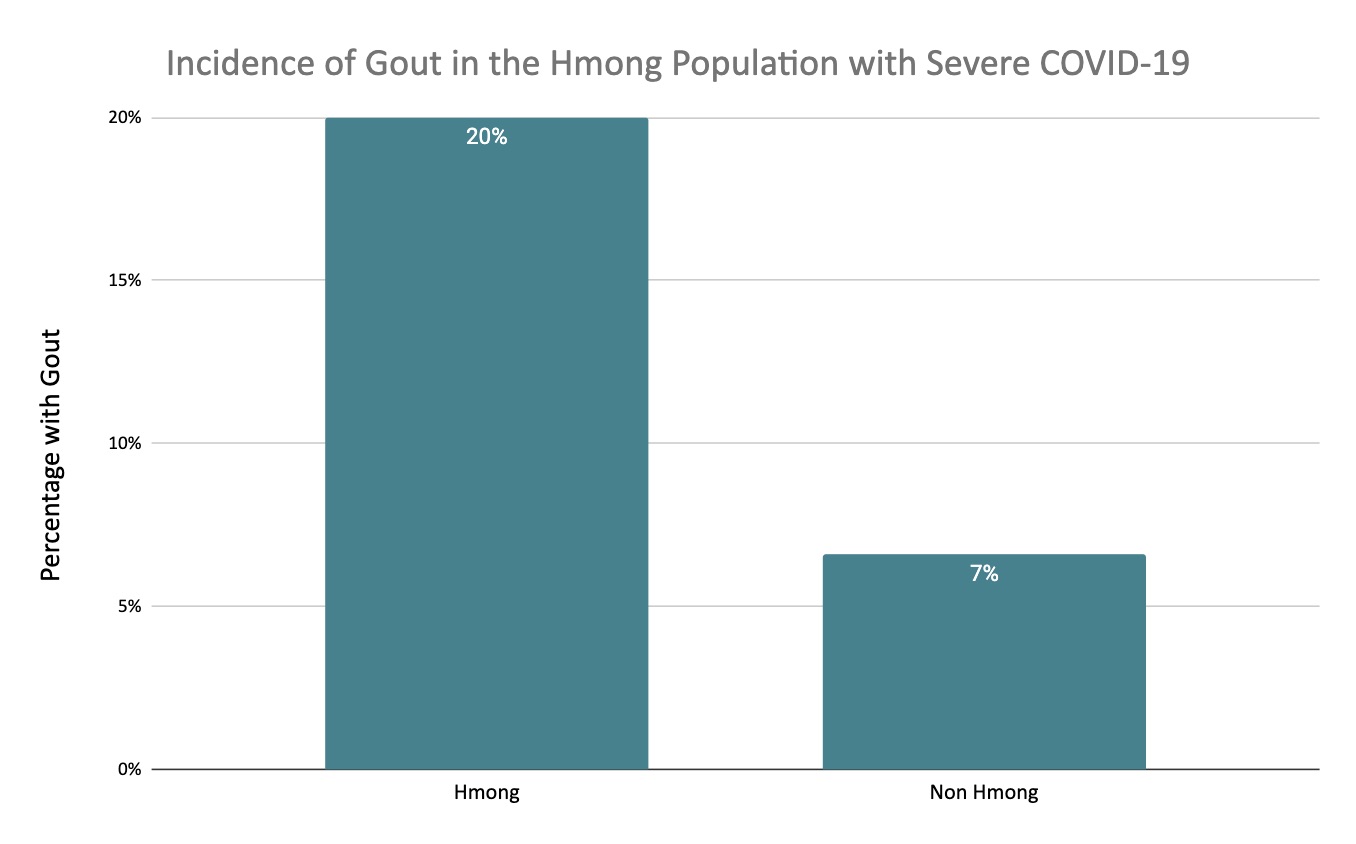
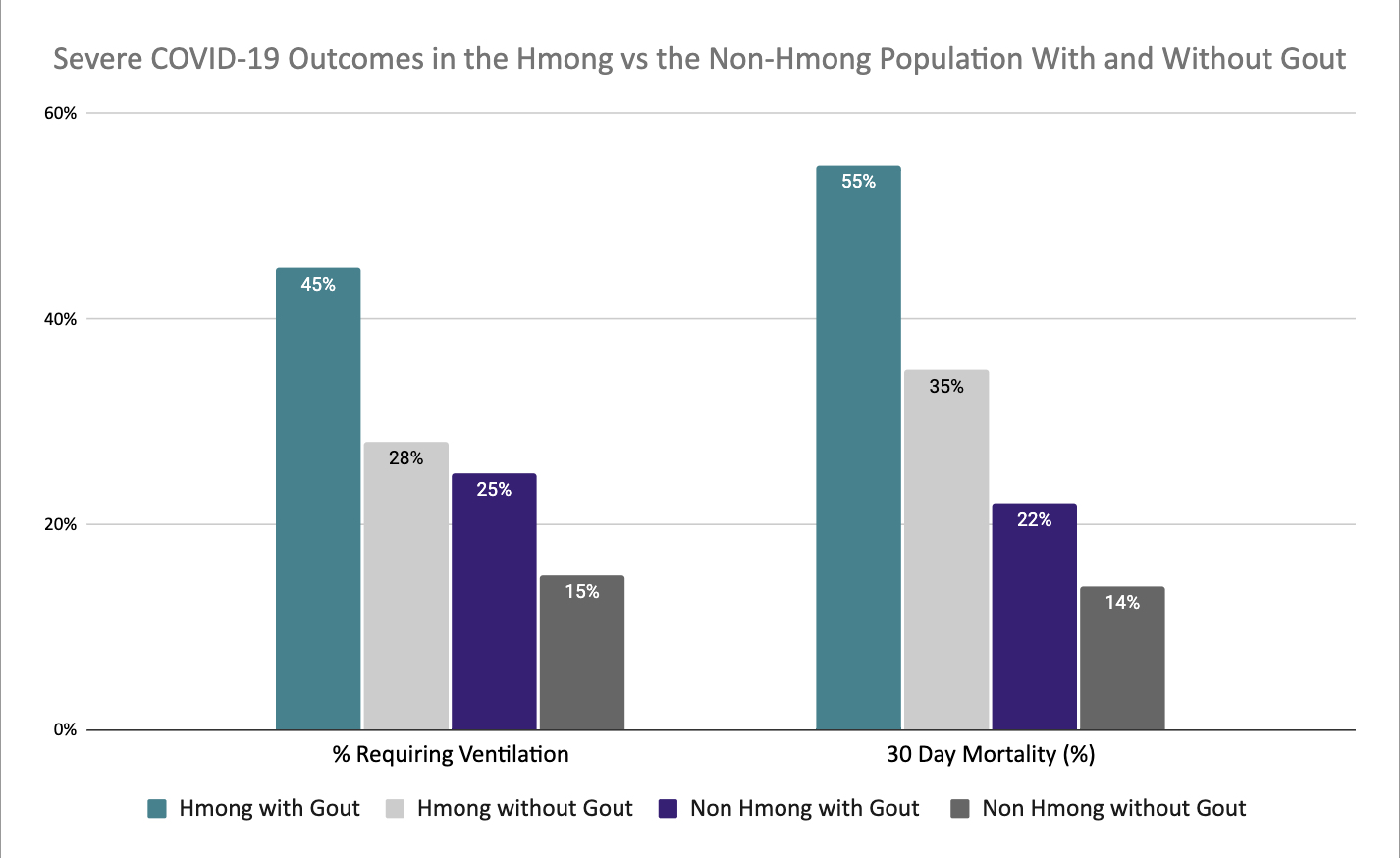
Results: From a cohort of 591 patients with severe COVID-19, 107 patients identified as Hmong. Among the total data set, 54 patients had a prior diagnosis of gout, with 22 of these patients identifying as Hmong. The prevalence of gout in the Hmong cohort was 20% versus 7% in the non-Hmong cohort with severe COVID-19 infection (Figure 1). The average age of the 22 patients with severe COVID-19 identifying as Hmong and with a comorbidity of gout was 62.9 years. Fourteen (63.6%) of these patients identified as male, with an average BMI of 28.7. Other underlying comorbidities for this cohort included chronic lung disease, chronic heart failure, renal disease, and diabetes with end organ damage (Table 1). The average length of stay was 12.2 days, with 10 patients requiring mechanical ventilation (45%). The 30-day mortality rate was 55% (n=12) (Figure 2). Demographics for the other cohorts are also displayed in Table 1. The other 85 patients who identified as Hmong without gout had the second highest ventilatory support needs (28%) and had a 35% 30 day mortality rate. In the non-Hmong gout cohort, 25% required invasive ventilatory support with a 30 day mortality rate of 22%. This is compared to the non-Hmong without gout cohort of which only 15% required mechanical ventilation and had a 14% 30 day mortality rate.
Conclusion: Our case series describes markedly severe COVID-19 outcomes in the Hmong population with gout with a 30-day mortality rate of 55%. Hmong patients without gout fared slightly better but still worse than non-Hmong patients with gout. The combination of genetic predisposition to hyperuricemia, the presence of gout, and the presence of COVID-19 infection was devastating in the Hmong population. These findings again highlight the comprehensive efforts needed in healthcare systems in approaching hyperuricemia and gout. Furthermore, in order to prevent future morbidity and mortality, there is a critical need for outreach and education to diverse ethnic and racial groups with gout due to the serious nature of the underlying disease process.
To cite this abstract in AMA style:
Falaas K, Schnaus M, Singer M, Hochstetler A, Khang P, Schmiechen K, Gertner E. Devastating Morbidity and Mortality Rates in the Hmong Population with a Diagnosis of Gout Who Had a COVID-19 Infection [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/devastating-morbidity-and-mortality-rates-in-the-hmong-population-with-a-diagnosis-of-gout-who-had-a-covid-19-infection/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/devastating-morbidity-and-mortality-rates-in-the-hmong-population-with-a-diagnosis-of-gout-who-had-a-covid-19-infection/