Session Information
Date: Tuesday, October 28, 2025
Title: (2015–2051) Miscellaneous Rheumatic & Inflammatory Diseases Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Sarcoidosis is a granulomatous multi-system disease with nervous system involvement in 5-20% of patients. Diagnosis of neurosarcoidosis is challenging due to its broad spectrum of phenotypic and radiographic manifestations. This study leverages a North American registry of patients misdiagnosed as neurosarcoidosis and provides a descriptive analysis of diagnostic tools used to evaluate patients for neurosarcoidosis.
Methods: Two hundred and forty-four patients with a diagnosis code of neurosarcoidosis were identified between 2010 and 2020 at a tertiary care academic institution. Chart review by a neurologist and rheumatologist identified 26 patients who were misdiagnosed as neurosarcoidosis and later found to have an alternative diagnosis. Twenty-three of these charts were reviewed to identify demographic data, relevant laboratory studies, neuroimaging, and pathology. Neuroimaging of a subgroup of 6 neurosarcoidosis mimics and 6 neurosarcoidosis controls were reviewed by 5 neuroimmunology specialists in a blinded survey to obtain additional data regarding radiographic diagnostic certainty of neurosarcoidosis and its mimics.
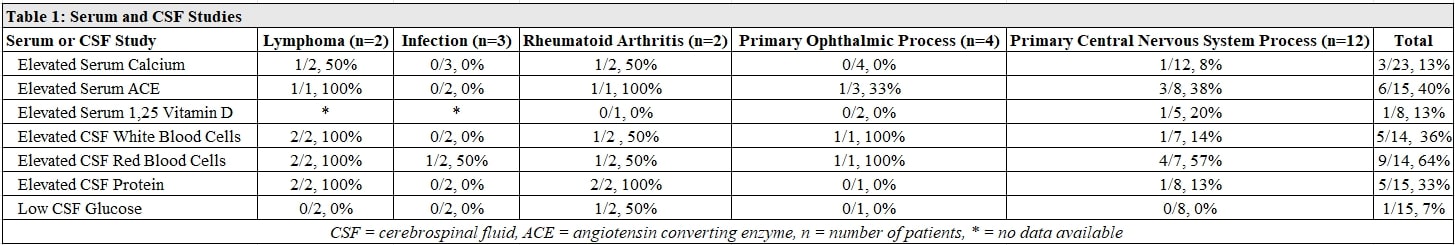
Results: Over half (52%) of the cohort was diagnosed with another primary CNS process, most commonly multiple sclerosis. Other common mimics included lymphoma (9%), infection (13%), primary ophthalmic conditions (17%), and rheumatoid arthritis (9%). Angiotensin converting enzyme (ACE) was elevated at least once in 40% of the patients. Cerebrospinal fluid (CSF) analysis showed an elevated white blood cell count and protein in approximately 1/3 of the cohort and low glucose in only 1 patient with rheumatoid arthritis. Of the 17 patients who had a biopsy of some tissue for their neurosarcoidosis workup, 12 had granulomas on pathology. Only 1 of 7 patients with a brain biopsy had granulomas on pathology. The majority of patients had MRIs of the brain and/or spine and the most common radiographic patterns were pachymeningeal and parenchymal enhancement.In a radiographic review survey of 6 neurosarcoidosis mimics and 6 neurosarcoidosis controls, 4 out of 6 mimics and 5 out of 6 controls were correctly identified based on group consensus. The idiopathic hypertrophic pachymeningitis (IHP) case and rheumatoid arthritis case were incorrectly diagnosed as neurosarcoidosis based on group consensus. One neurosarcoidosis control was felt to be most likely IgG4-related disease (IgG4-RD) by 2 reviewers and neurosarcoidosis by 2 reviewers. Pre-existing knowledge of a pulmonary sarcoidosis diagnosis appeared to influence diagnostic certainty of neurosarcoidosis.
Conclusion: Common mimics of neurosarcoidosis include infection, lymphoma, rheumatoid arthritis, another CNS process, and primary ophthalmic processes. Laboratory and CSF studies may not be sensitive for neurosarcoidosis. MRI review by a neurosarcoidosis specialist can help differentiate neurosarcoidosis from mimics with radiographic differences, such as infection or multiple sclerosis, and spare the patient a biopsy. Biopsy may be needed to distinguish neurosarcoidosis from diseases that are radiographically similar, such as IHP or IgG4-RD. Limitations include small sample size and limited follow-up.
To cite this abstract in AMA style:
Rangaswamy S, Lopez A, Sugita M, Eyman E, Lackey E, Shen J. Descriptive Analysis of a Cohort of Neurosarcoidosis Mimics [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/descriptive-analysis-of-a-cohort-of-neurosarcoidosis-mimics/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/descriptive-analysis-of-a-cohort-of-neurosarcoidosis-mimics/

.jpg)
.jpg)