Session Information
Date: Monday, November 18, 2024
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Kawasaki disease shock syndrome (KDSS) is a phenotype of Kawasaki disease (KD) associated with higher rates of refractory KD (RKD) and coronary artery aneurysms (CAAs). The pathophysiology of KDSS is incompletely understood and may overlap with other similar hyperinflammatory conditions such as multisystem inflammatory syndrome in children (MIS-C). We describe RKD patients diagnosed with KDSS at a large tertiary center and compare them to patients with non-shock refractory KD to identify unique clinical and laboratory features.
Methods: With IRB approval, we performed a retrospective chart review of patients diagnosed with RKD, i.e. those requiring treatment after initial IVIG, at our institution from 2017-2019. KDSS patients defined by hypotension on admission or requiring > 60 mL/kg of fluid resuscitation or vasopressors were identified. Demographics, clinical features, diagnostic findings, treatment, and outcomes were collected.
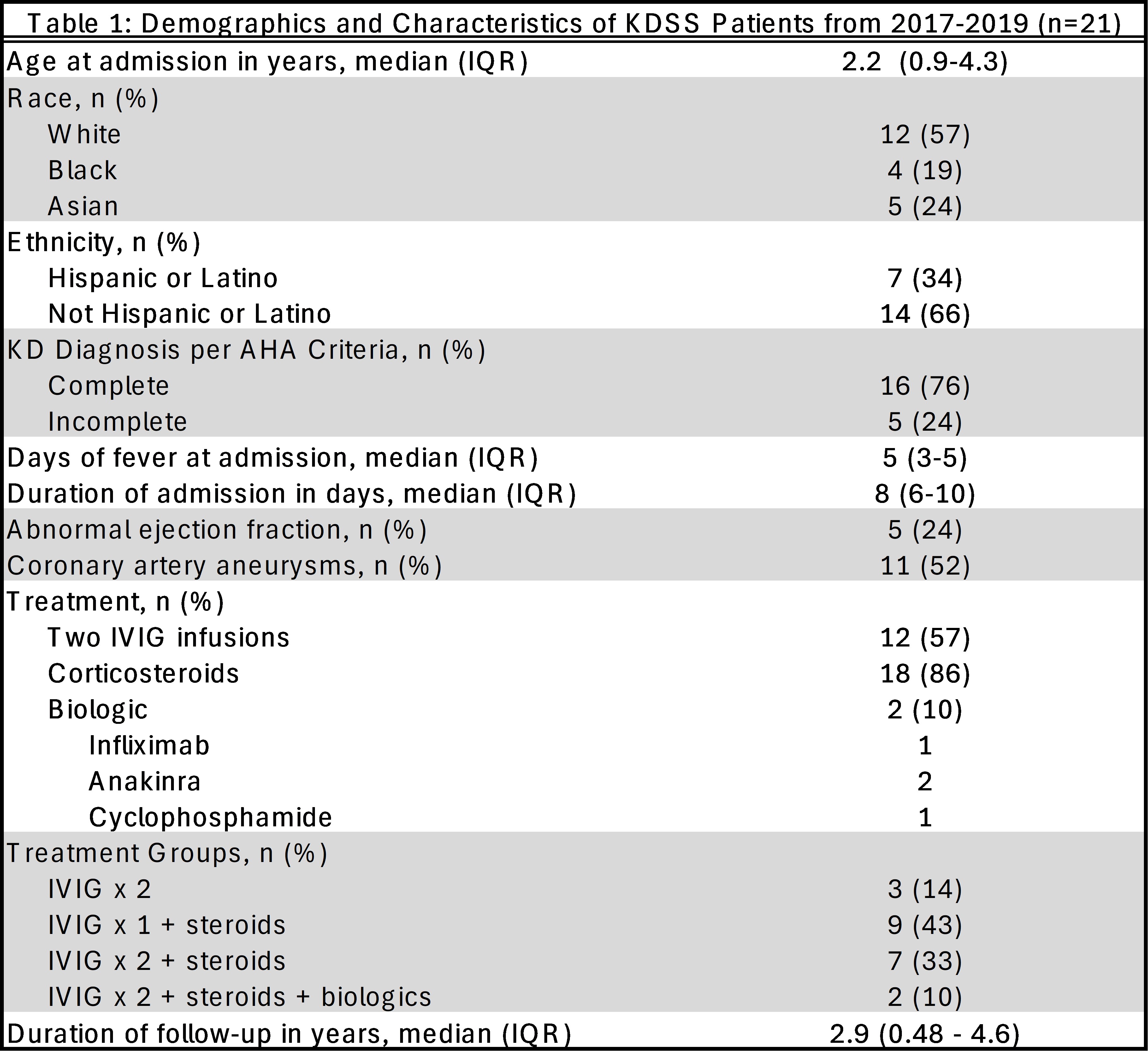
Results: Out of 103 patients diagnosed with RKD, 21 (20%) were diagnosed with KDSS and there were no significant demographic differences (Table 1). The median age of patients with KDSS was 2.2 years (IQR 0.9-4.3). Per American Heart Association (AHA) criteria, 16 (76%) had complete KD while 5 (24%) had incomplete KD. Five (24%) KDSS patients had myocardial dysfunction with depressed or low-normal ejection fraction compared to 2 (2%) in the non-shock RKD group. Eleven (52%) KDSS patients had CAAs throughout their course with 7 developing small, 3 medium, and 1 giant CAAs which was similar to the non-shock RKD patients. The additional immunomodulatory treatment KDSS patients received after their initial IVIG infusion included 12 (57%) with second infusion of IVIG, 18 (86%) with corticosteroids, and 2 (10%) with biologic therapy. Only 3 KDSS patients (14%) were treated with two infusions of IVIG alone.
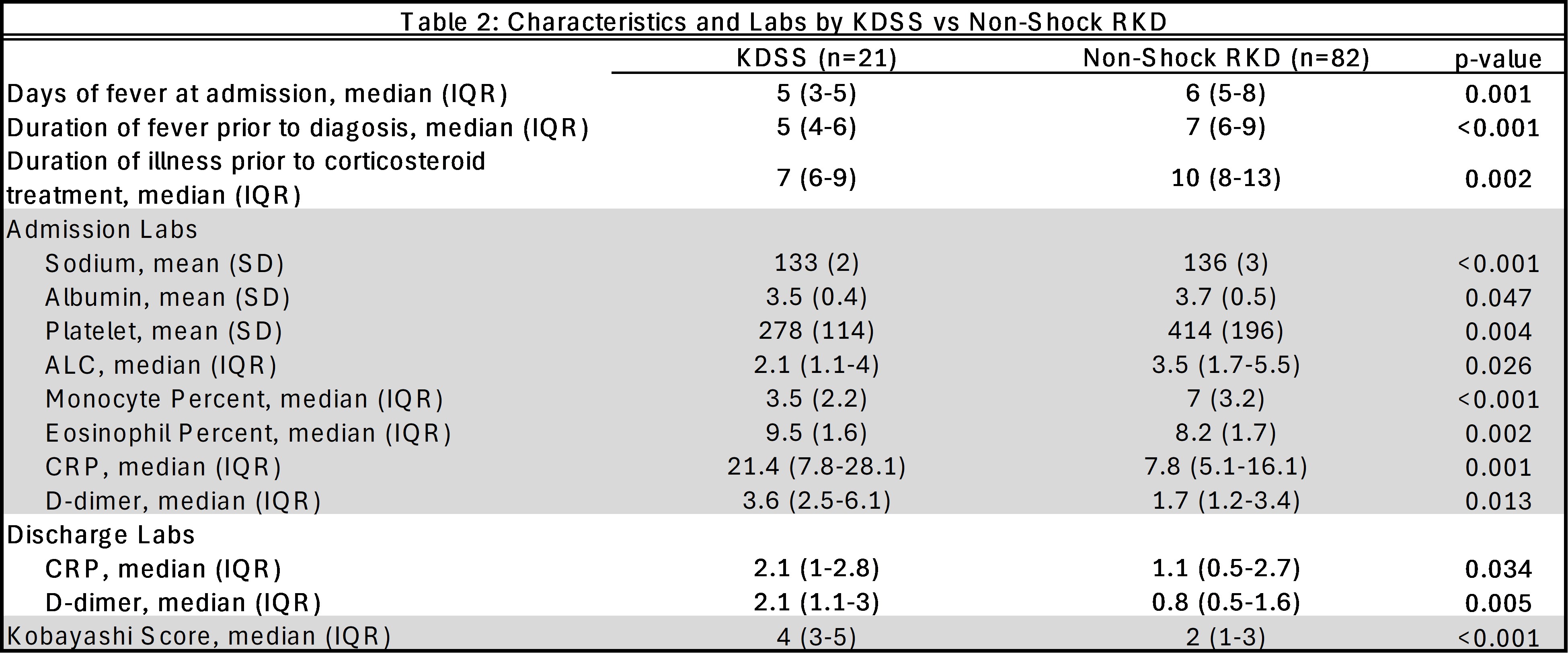
KDSS patients had shorter durations of fevers/illness prior to admission, to their diagnosis of KD, and to steroid treatment compared to other RKD patients (p < 0.05). A lower sodium, albumin, platelet, absolute lymphocyte count, monocyte and eosinophil percentage on admission were associated with KDSS (p < 0.05). KDSS patients had significantly higher Kobayashi scores (p < 0.001) and CRP and d-dimer on admission and discharge compared to non-shock RKD (p < 0.05). There were no significant coronary artery aneurysm differences between patients with KDSS and non-shock RKD.
Conclusion: KDSS patients in this cohort have shorter illness duration before diagnosis and treatment, possibly preventing significant worsening of coronary artery abnormalities compared to non-shock RKD. Among the laboratory parameters that differ between patients with KDSS and non-shock RKD, significantly elevated CRP and d-dimers at discharge suggest a prolonged inflammatory phase of disease.
To cite this abstract in AMA style:
Nguyen J, Guffey D, Ramirez A, Lai J, Vogel T, Sexson Tejtel S, Yildirim-Toruner C, De Guzman M. Description of Patients with Kawasaki Disease Shock Syndrome at a Large Tertiary Center [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/description-of-patients-with-kawasaki-disease-shock-syndrome-at-a-large-tertiary-center/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/description-of-patients-with-kawasaki-disease-shock-syndrome-at-a-large-tertiary-center/