Session Information
Date: Saturday, November 6, 2021
Title: Health Services Research Poster I: Lupus, Inflammatory Arthritis, & More (0128–0148)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Systemic sclerosis interstitial lung disease (SSc-ILD) and pulmonary hypertension (SSc-PH) are leading causes of morbidity and mortality in patients with SSc. Few screening guidelines exist to identify patients early in their disease course. The aim of this study is to characterize a cohort of patients diagnosed with SSc, compare their lung disease risk to that of a subset of the EUSTAR cohort, and better understand screening practices for SSc by rheumatologists in our medical center.
Methods: We conducted a retrospective analysis of patients with SSc at a rural academic medical center. We identified patients 18 years and older with a SSc diagnosis (via ICD-9 and -10 codes) and seen by a rheumatologist between 01/01/2018 and 12/31/2020. We reviewed pulmonary function tests (PFTs) and transthoracic echocardiogram (TTE) orders between 01/01/2017 and 12/31/2020 for monitoring, focusing on diffusion capacity (DLCO) and pulmonary artery systolic pressure (PASP). Patients were defined as having PH if their PASP was >36.0 or if the TTE report stated evidence of PH. We compared the mean DLCO and PASP values to the EUSTAR subset using a two-sample t-test with unequal variance, age using a two-sample t-test with equal variances, and percent female patients using a Pearson’s chi-square test. Statistical significance was defined as p< 0.05. Rheumatologists were invited to participate in an online, self-administered survey of 15 questions about PFT and TTE ordering practices and physician behaviors regarding abnormal results.
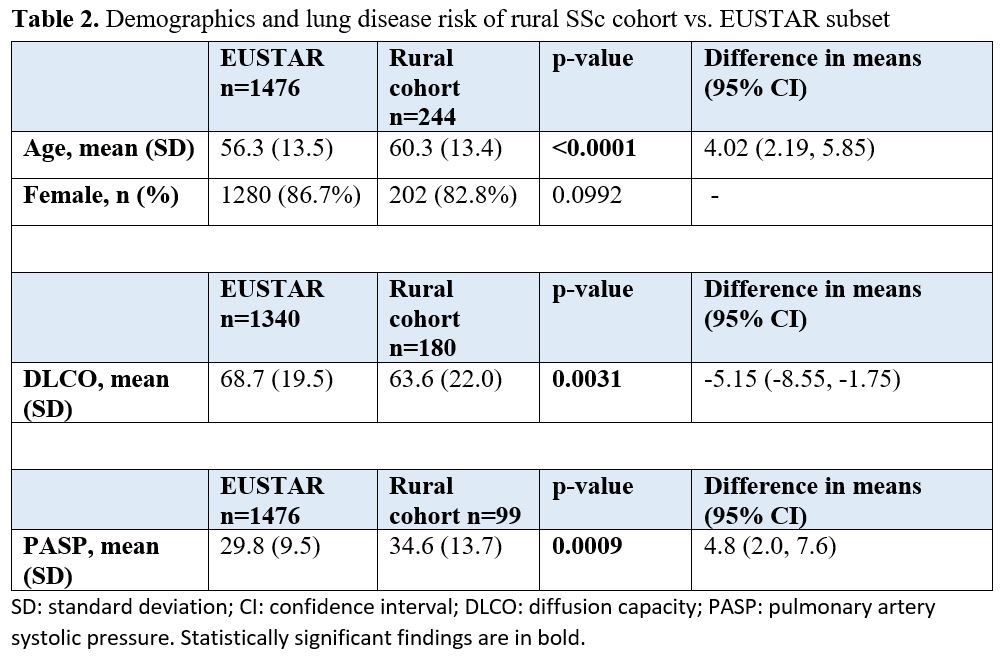
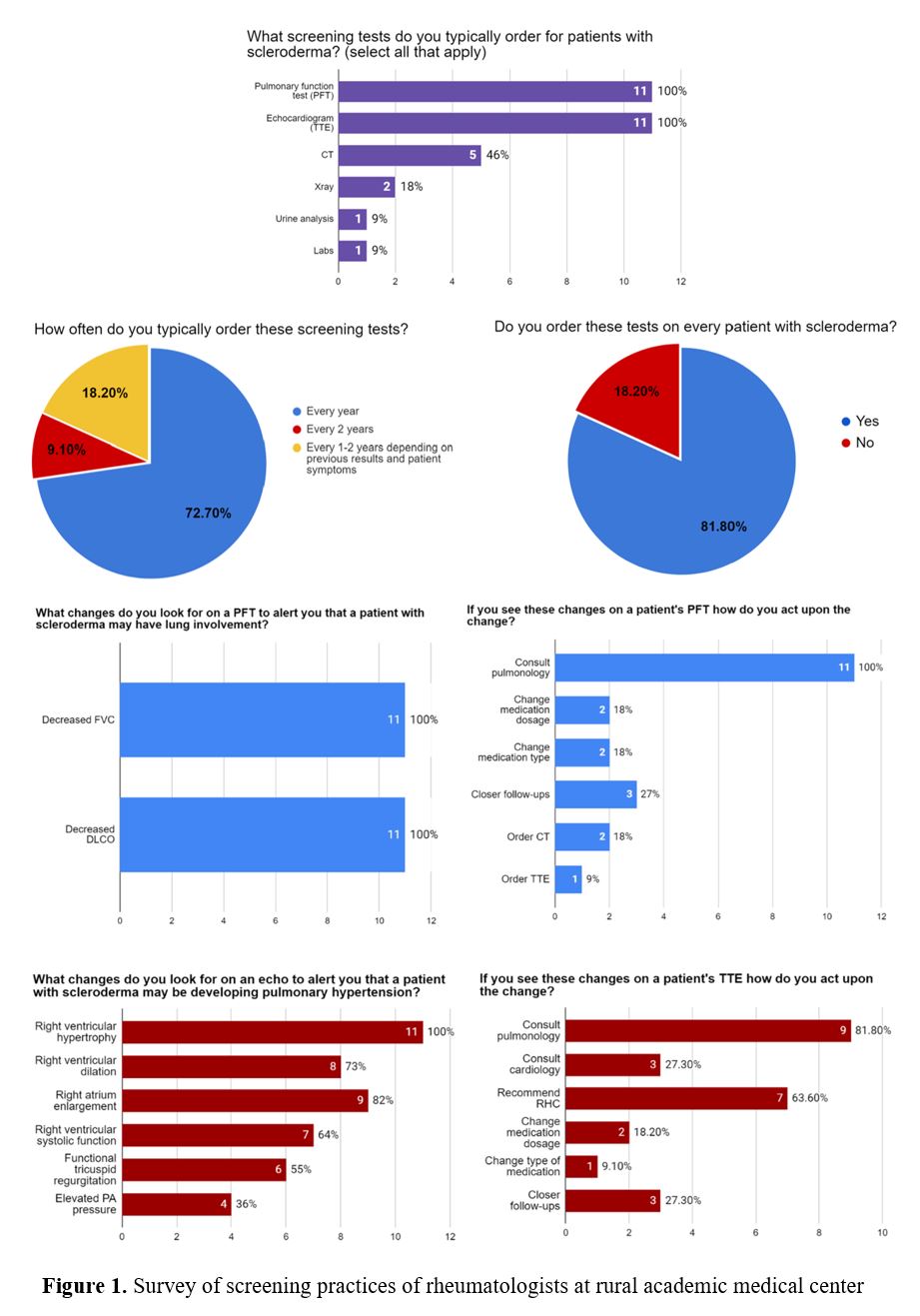
Results: A total of 244 patients with a SSc diagnosis were seen in a 3-year period, with 187 (over 75%) patients having a visit in the last year. Please see Table 1 for demographic data. 181 patients (74.2%) had PFTs completed. Of those completed, the average DLCO was 63.6% and 20% of patients had a DLCO less than 50%. For TTEs, 189 patients (77.5%) had TTEs ordered with 3 incomplete tests. Of interest, only 99 (53%) had a reported PASP value, and mean PASP was 34.6mmHg (Table 1). Compared to EUSTAR, patients were older (60.3 vs. 56.3 years; p< 0.0001) and mean DLCO values were lower (63.6% vs. 68.7%; p=0.0031). Mean PASP comparatively was 34.6 mmHg vs. 29.8 mmHg (p=0.0009) (Table 2). The self-administered survey had a completion rate of 84.6% with 11 of 13 physicians electing to participate. Please see Figure 1 for survey results.
Conclusion: We identified an opportunity for early detection of SSc-ILD and SSc-PH in scleroderma patients within our academic health system. This would be achieved by improving ordering practices of PFTs and TTE for scleroderma monitoring. Additionally, we identified our population as, statistically, having potentially more severe disease compared to the EUSTAR cohort. We intend to investigate these findings further and explore clinical and social factors possibly playing a role in disease progression. We are hoping to institute improvements in best practice and develop EHR toolkits to improve monitoring of our SSc patients in the future.
To cite this abstract in AMA style:
Marinock J, Nicholas P, Koons K, Kriplani R, Berger A, Bulbin D. Description of a Scleroderma Cohort and Management of Lung Disease Risk at a Rural Academic Medical Center [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/description-of-a-scleroderma-cohort-and-management-of-lung-disease-risk-at-a-rural-academic-medical-center/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/description-of-a-scleroderma-cohort-and-management-of-lung-disease-risk-at-a-rural-academic-medical-center/