Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Nailfold capillaroscopy (NFC) is an essential tool for evaluating microvascular abnormalities in patients with Raynaud’s phenomenon (RP) in United States (U.S.) Veterans (1). While dermatoscopy is an acceptable and cost-effective screening method for nailfold assessment in systemic sclerosis (SSc), published guidelines highlight the importance of clear image acquisition for appropriate interpretation (2). The objective of this project was assessment of NFC in patients with concern for connective tissue disease (CTD)-related RP to determine whether different intensities of skin pigmentation impacts the interpretability of dermatoscopy screening.
Methods: Patients undergoing evaluation for CTD-related RP were consented for participation in Institutional Review Board approved research at the time of care at the Veterans Affairs (VA) Hospital (No. 1618579-17). Patients were prepared for NFC per published protocols (3). Images were obtained with two devices available at the VA Hospital, a dermatoscope attached to a smart phone (200X magnification, smart phone focus) and Smart G-Scope (250X magnification, USB automatic focus). Each image was classified for the clarity of image by two capillaroscopy experts. Microvascular findings for capillary density, apical enlargement, hemorrhages, and abnormal shapes were determined by the capillarscopy.io software application.
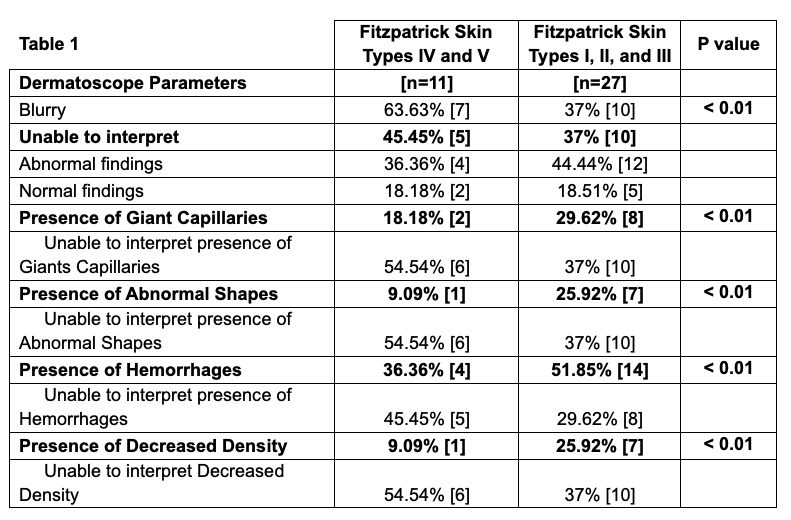
Results: A total of 38 U.S. Veterans were assessed for RP by NFC using clinically available two devices. Among these, 28% (n=11) of subjects were classified as African American. As shown in Table 1, dermatoscopy produced blurry images in 63.6% (7/11) of patients with Fitzpatrick skin type IV and V and 37% (10/31) in Fitzpatrick skin type I, II, and III. In 45.5% (5/11) of dermatoscopy exams in Fitzpatrick skin type IV and V skin were deemed uninterpretable compared to 37% (10/31) of Fitzpatrick skin type I, II, and III (kappa statistic >0.9). Smart G-Scope improved interpretability across the cohort of patients (Table 2), especially in Fitzpatrick Skin Types IV and V. A scleroderma (SD)-pattern characteristic of scleroderma microangiopathy was detected by the Smart-G-scope in 3 of those 5 uninterpretable dermatoscope acquired images (Table 3).
Conclusion: In patients with CTD-related RP, particularly among African American Veterans, a dermatoscopy device led to a high rate of uninterpretable examinations. The Smart-G USB device improved diagnosis of abnormal NFC. These results highlight that reliance on dermatoscopy alone as a screening tool may risk underdiagnosing microvascular involvement in SSc.References:1. Frech TM et al. BMC Rheumatol. 2021; 15; 5 (1): 42. 2. Radic M et al. Clin Exp Rheumatol. 2020; 38 Suppl 125 (3): 132-136. 3. Smith V et al. Autoimmun Rev. 2020; 9 (3): 102458.
.jpg) Table 2: Nailfold capillaroscopy characteristics
Table 2: Nailfold capillaroscopy characteristics
.jpg) Table 3: Capillaroscopy findings in the uninterpretable group.
Table 3: Capillaroscopy findings in the uninterpretable group.
To cite this abstract in AMA style:
Maldonado G, Cutolo M, Frech T, Radic M, Snow M, Smith V. Dermatoscopy Limitation and the Critical Role of Capillaroscopy in Systemic Sclerosis and Raynaud’s Phenomenon among African American Veterans [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/dermatoscopy-limitation-and-the-critical-role-of-capillaroscopy-in-systemic-sclerosis-and-raynauds-phenomenon-among-african-american-veterans/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/dermatoscopy-limitation-and-the-critical-role-of-capillaroscopy-in-systemic-sclerosis-and-raynauds-phenomenon-among-african-american-veterans/