Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Diagnoses of depression, highly prevalent in SLE and RA populations, were associated with increased cardiovascular disease (CVD) risk in the All of Us Research Program. Here we examine CVD risks associated with alternate ways of identifying depression and depression risk in this large US-wide electronic health record (EHR) cohort of SLE and RA patients using: 1) diagnostic codes, 2) antidepressant use, and 3) depression polygenic risk score (depPRS). We examined each in relation to CVD event risks in an SLE and RA cohort over time, hypothesizing that diagnosed depression and antidepressant use would be more strongly associated with CVD than would genetic susceptibility to depression.
Methods: All of Us (version 7) includes >287,000 adult US participants who gave consent for linkage to their EHRs, >230,000 of whom provided blood for whole genome sequencing. RA and SLE patients were identified by ≥2 ICD-9, ICD-10, or SNOMED codes >2 months apart within 2 years of enrollment. We excluded patients with CVD at baseline. Genetic risk for depression was defined as in the top 20% of a published multiethnic depPRS (Meng X et al Nat Genet. 2024). Major depression was identified by ≥2 baseline ICD-9/10 or SNOMED codes. Depression treatment was defined by any baseline antidepressant medication (tricyclic antidepressants, serotonin reuptake inhibitors, atypical antidepressants). For each measure of depression, a Cox model estimated hazard ratio (HR) for incident CVD risk in SLE and RA patients from enrollment. The primary outcome was a composite of acute MI, percutaneous coronary intervention (PCI), coronary artery bypass graft (CABG) or stroke (ICD9/10, SNOMED codes). Patients were followed until 1st CVD event, 5 years, or data end (7/2022). Covariates included age, sex, race, ethnicity, income, educational level, smoking status, obesity and comorbidities. (Sample size for depGRS was 36% smaller as not all had genetic data.)
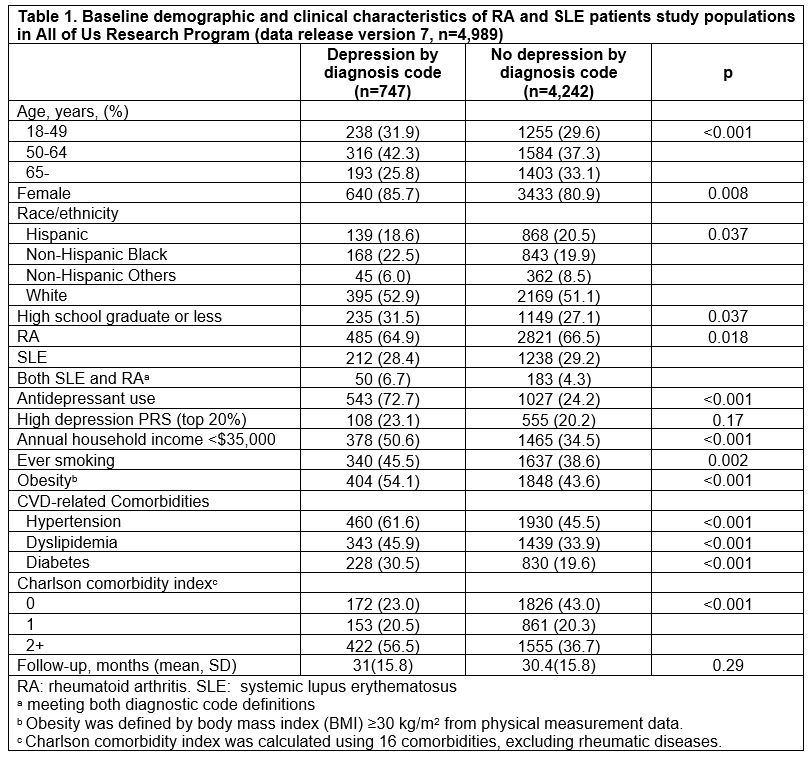
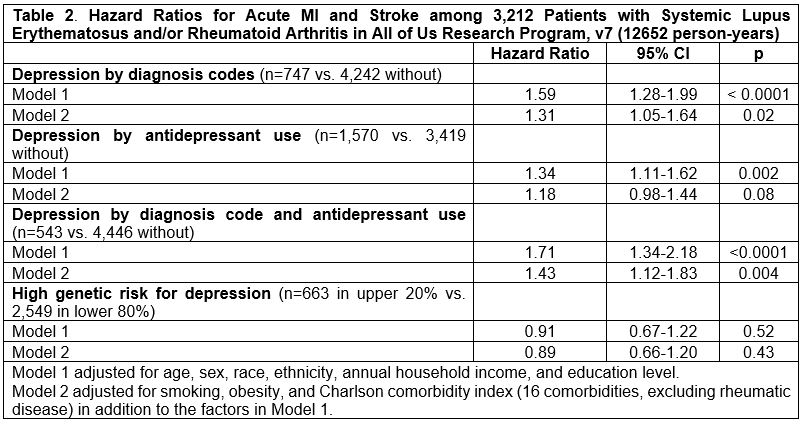
Results: We included 3,539 patients with RA, 1,683 with SLE (including 233 with both). Baseline characteristics by depression by diagnostic codes are in Table 1. Those with depression diagnoses were less educated, had lower income, smoked more, were more obese, and had more comorbidities. Patients were followed for mean 30.4 months (SD 15.8). HRs for acute MI and stroke were higher among patients with versus without diagnosed depression and antidepressant use than genetic depression risk (Table 2). After adjustment for smoking status, obesity, and Charlson comorbidity index, HRs (95% confidence intervals) for CVD events in patients with diagnosed depression were 1.31 (1.05-1.64), treated depression 1.18 (0.98-1.44) and genetic depression risk 0.89 (0.66-1.20).
Conclusion: In this large diverse U.S. cohort of patients with SLE and/or RA without prior CVD events, depression identified by diagnosis codes or by receipt of antidepressant medication was more strongly associated with increased risk of incident CVD event than was having a high genetic depression risk score. Findings suggest that diagnosed and treated depression are more strongly related to CVD risk than is genetic susceptibility to depression among SLE and RA patients.
To cite this abstract in AMA style:
Cui J, Yee J, Oakes E, Karlson E, Santacroce L, Guan H, Kubzansky L, Koenen K, Feldman C, Costenbader K. Depression Genetic Risk, Diagnoses, and Treatments in Association with Cardiovascular Disease Events Among Patients with Systemic Lupus Erythematosus and Rheumatoid Arthritis in the All of Us Research Program [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/depression-genetic-risk-diagnoses-and-treatments-in-association-with-cardiovascular-disease-events-among-patients-with-systemic-lupus-erythematosus-and-rheumatoid-arthritis-in-the-all-of-us-research/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/depression-genetic-risk-diagnoses-and-treatments-in-association-with-cardiovascular-disease-events-among-patients-with-systemic-lupus-erythematosus-and-rheumatoid-arthritis-in-the-all-of-us-research/