Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Diagnostic delay in axial spondyloarthritis (axSpA) presents a challenge in the management of the condition, despite increased awareness. Reducing the gap between symptom onset and time of diagnosis is needed to limit associated morbidity and mortality. We aimed to examine delay to diagnosis in a large cohort of well characterised individuals with axSpA, with the specific objectives of:
- Assessing if delay to diagnosis has reduced in individuals with more recent onset of disease
- Identifying clinical and demographic characteristics associated with delayed diagnosis
- Determining whether sex has an impact on delay to diagnosis
- Assessing the association between delay to diagnosis and disease severity.
Methods: The Ankylosing Spondylitis Registry of Ireland (ASRI) provided the cohort for this study. The objectives of ASRI are to provide descriptive epidemiological data on the Irish axSpA population. A standardised clinical assessment is performed on each patient. Structured interviews provide patient-reported data. Delay to diagnosis was calculated as age at diagnosis minus age at symptom onset. Validated outcome measures were collected: Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), Bath AS Functional Index (BASFI), Health Assessment Questionnaire (HAQ), AS Quality of Life (ASQoL), and Bath AS Metrology Index (BASMI).
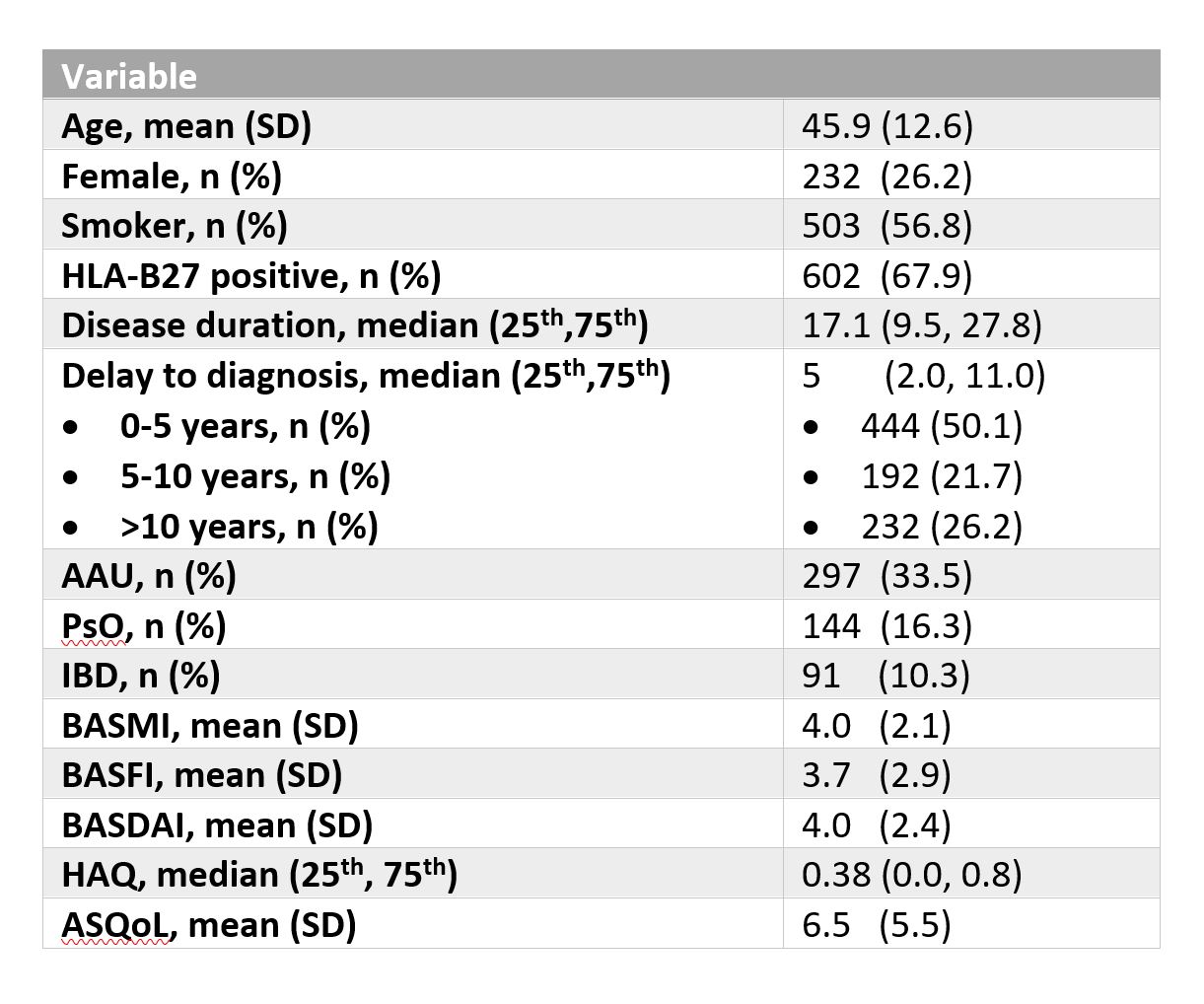
Results: Eight hundred and eighty-six patients were included, 644 of whom were male (73%), mean age 46 years (SD 13) and 76% (n=667) fulfilled modified New York (mNY) criteria. Detailed baseline clinical and demographic characteristics are outlined in Table 1.
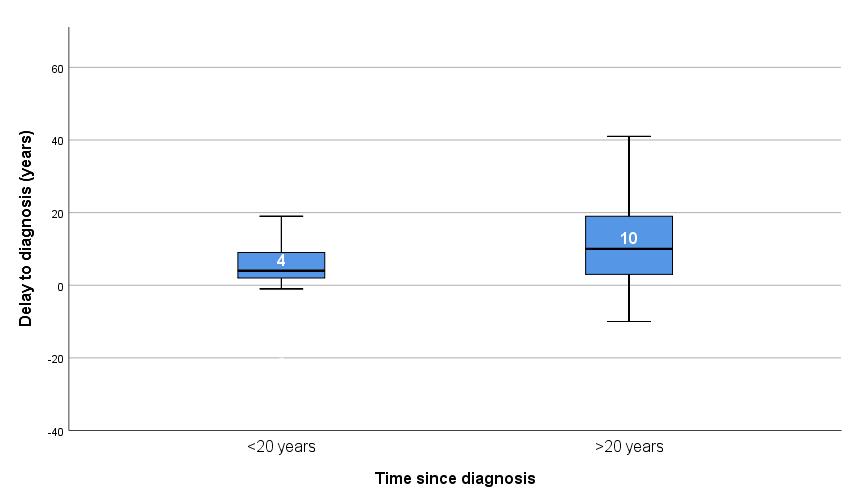
The mean (SD) disease duration was 19 (12) years, with 27% having a duration of less than 10 years, 32% having duration of 10-20 years and 42% with a duration of >20 years. The median delay to diagnosis in the whole cohort was 5 years (2, 11), with 51% (n=444) of the cohort diagnosed within 5 years, 22% (n=192) diagnosed between 5-10 years and 27% (n=232) diagnosed more than ten years from symptom onset. The median delay to diagnosis has reduced significantly (< 0.01) in recent years (see Figure 1).
Factors associated with a shorter delay to diagnosis include smoking (6.7 vs 8.9 years, p< 0.01), peripheral arthritis (7.0 vs 8.4 years, p=0.02) and absence of sacroiliitis on x-rays (6.5 vs 8.4 years, p=0.03). HLA-B27 status had no impact on delay to diagnosis and there was no difference between sexes. The presence of EAM did not influence the delay to diagnosis.
When compared to a delay of < 5 years, individuals with a delay to diagnosis > 10 years had significantly higher BASMI (4.7 vs 4.0, p=0.01) and BASFI (4.8 vs 3.8, p=0.02) scores, with no difference in BASDAI (4.1 vs 3.9, p=0.6).
Conclusion: Although still present, delay to diagnosis has reduced in individuals with a more recent diagnosis of axSpA, with no sex effect seen. Longer delays to diagnosis are associated with more severe disease in this cohort, indicating a significant unmet need in the management of axSpA.
To cite this abstract in AMA style:
McWalter M, MacGearailt C, Maguire S, O'Shea F, Fitzgerald G. Delay to Diagnosis in Axial Spondyloarthritis: The Gap Is Closing, but Persistent Association with Severe Disease [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/delay-to-diagnosis-in-axial-spondyloarthritis-the-gap-is-closing-but-persistent-association-with-severe-disease/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/delay-to-diagnosis-in-axial-spondyloarthritis-the-gap-is-closing-but-persistent-association-with-severe-disease/