Session Information
Date: Sunday, November 12, 2023
Title: (0609–0672) Systemic Sclerosis & Related Disorders – Clinical Poster I: Research
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Prior studies have shown an increased risk of malignancy in patients with systemic sclerosis (SSc). The reasons for this increased risk may be multifactorial, including effects of chronic inflammation, genetics, shared environmental risk factors, use of immunosuppressive medications, among others. The aim of this study is to identify and characterize malignancy risk factors in a diverse SSc cohort.
Methods: A retrospective cohort was assembled of all patients with SSc followed within a large, urban, tertiary care center. Validated ICD codes were used to identify cases. Descriptive statistics were used to study the cross-sectional distribution of patient characteristics, including age, sex, ethnicity, health insurance status, smoking status, scleroderma subtype, mycophenolate (MMF) use and other immunosuppressant use. Student t-test was performed to compare variations in age. Chi-square test and Fisher exact test were used to examine the difference in other categorical characteristics of patients with and without malignancy. The prevalence of specific types of cancers was calculated. Odds ratios (OR) of cancer diagnosis with respect to patient characteristics were calculated with multivariable logistic regression.
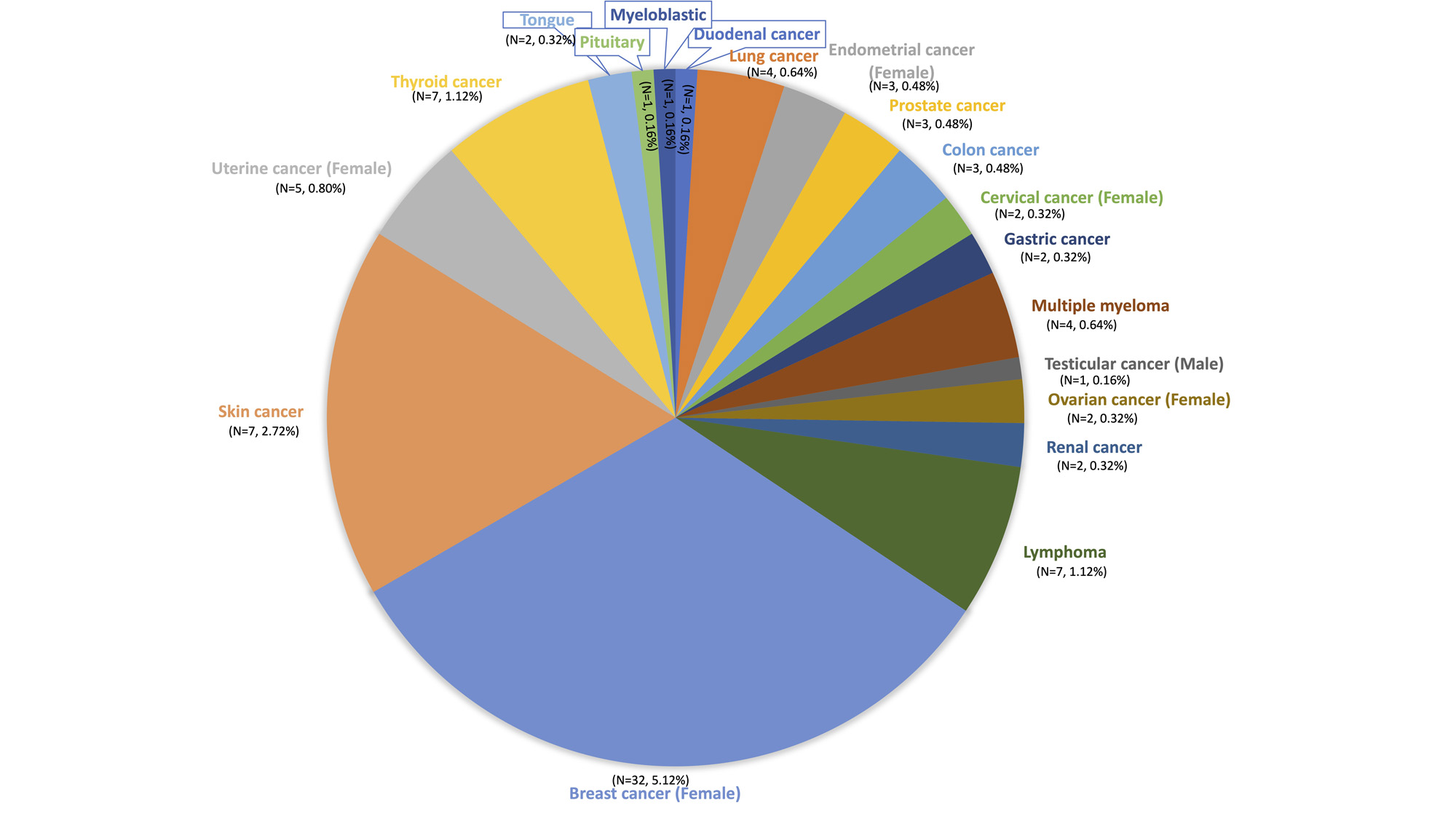
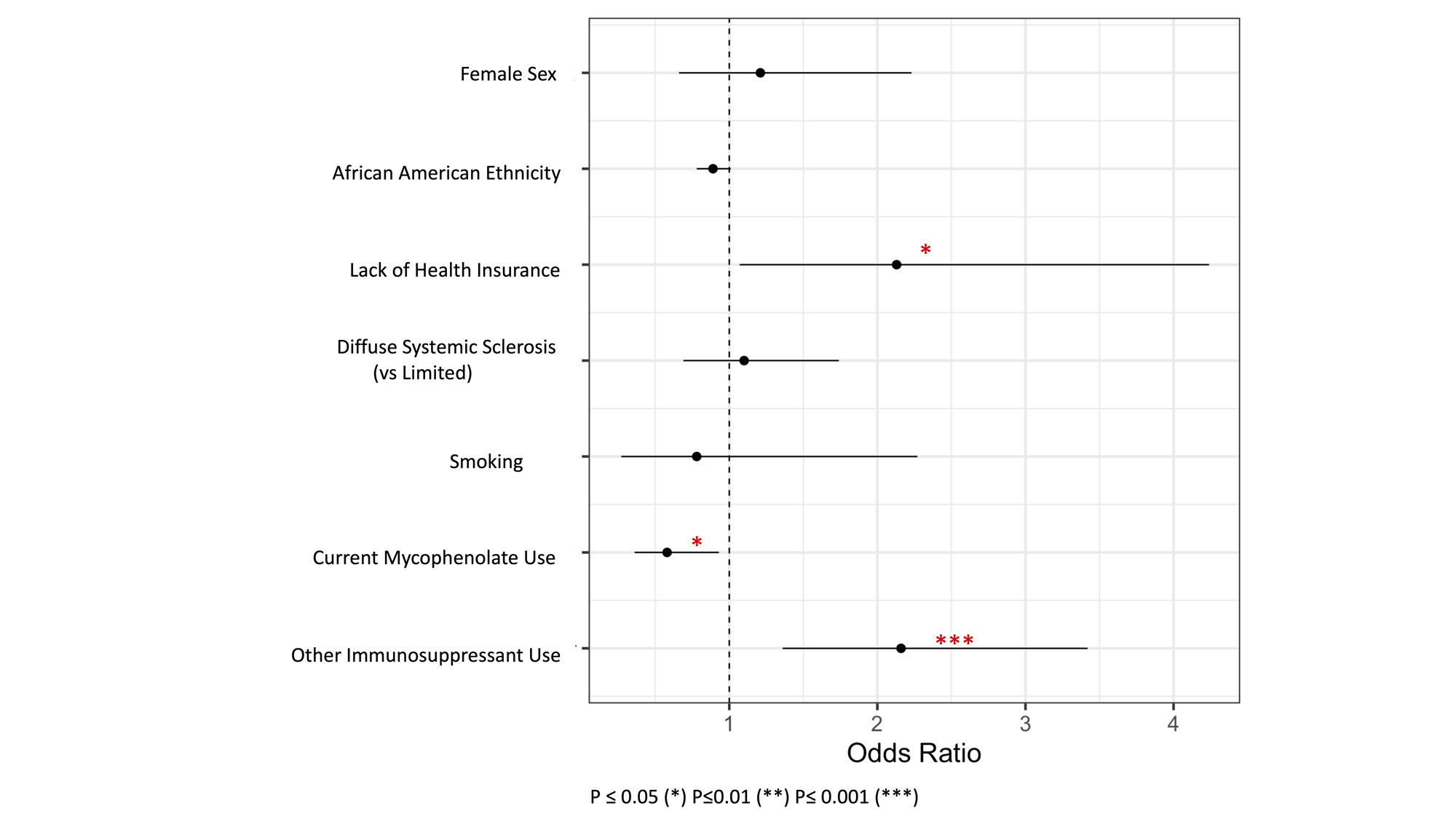
Results: A total of 625 patients met inclusion criteria. The distribution of participant characteristics was calculated and stratified by cancer diagnosis (Table 1). 93 (14.9%) patients were found to have a history of cancer. Breast cancer (N=32, 5.1%) was the most prevalent cancer in our cohort; distribution of each specific malignancy is outlined in Figure 1. Patients with a malignancy history were older than those without malignancy (median age 69 vs 61 P < 0.01). Lack of medical insurance was associated with increased odds of malignancy (OR 2.13, 95% CI 1.07-4.24, P = 0.03). Participants taking MMF were significantly less likely to be diagnosed with malignancy (OR 0.58, 95% CI 0.36-0.94, P = 0.03), whereas other immunosuppressant use was associated with higher prevalence of malignancy (OR 2.16, 95% CI 1.36-3.43, P = 0.001) (Figure 2). The multivariable logistic regression showed cancer had statistically significant associations with public insurance (P = 0.01), lack of insurance(P = 0.01), MMF (P< 0.01), and other immunosuppressants (P< 0.01), but not with SSc’s time of diagnosis, SSc subtypes, or smoking.
Conclusion: While MMF has been associated with increased malignancy risk in prior studies, this analysis showed a reduced odds of malignancy in participants with SSc treated with mycophenolate. The reason for this unexpected finding is unclear and further studies are warranted to determine if a relationship exists beyond correlation. Lack of health insurance, increasing age and non-MMF immunosuppressant use are associated with increased malignancy risk in this urban, single-center multiethnic SSc cohort. The cancer prevalence in our cohort is similar to prior SSc studies, and higher than the general population.
To cite this abstract in AMA style:
Feng J, Dobrowolski C, He C, Verma H, Vasoya R, Qian D, olumuyide E, Leong A, Menand J, Bastos Silva M, Courant V, Lutgen S. Decreased Odds of Malignancy with Mycophenolate Use in a Single-Center Scleroderma Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/decreased-odds-of-malignancy-with-mycophenolate-use-in-a-single-center-scleroderma-cohort/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/decreased-odds-of-malignancy-with-mycophenolate-use-in-a-single-center-scleroderma-cohort/