Session Information
Session Type: Abstract Session
Session Time: 4:00PM-5:30PM
Background/Purpose: Biologic disease modifying anti-rheumatic drugs (bDMARDs) such as anti-tumor necrosis factors(anti-TNFs) improve clinical and radiographic outcomes in rheumatoid arthritis (RA). However, their use is associated with dose- and age-dependent adverse effects including increased risk of serious infections. In recent years, de-escalation (or deprescribing or tapering/discontinuing) has been proposed as an approach to reduce polypharmacy and optimize medication use in older adults more prone to the negative, often additive, adverse effects of medications. Current clinical practice guidelines recommend de-escalating bDMARDs in RA patients with low disease activity or in remission. We evaluated the prevalence of and factors associated with anti-TNF de-escalation among Medicare beneficiaries with RA in usual care.
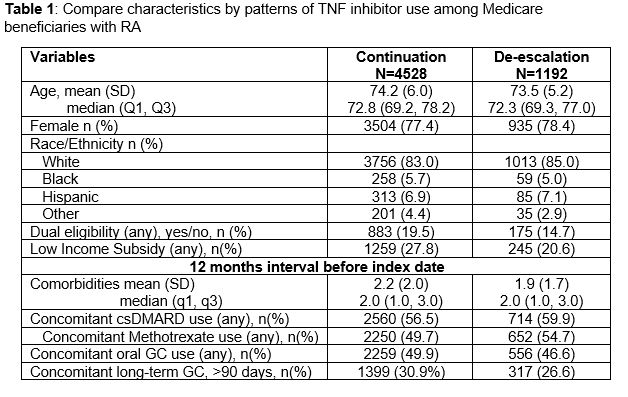
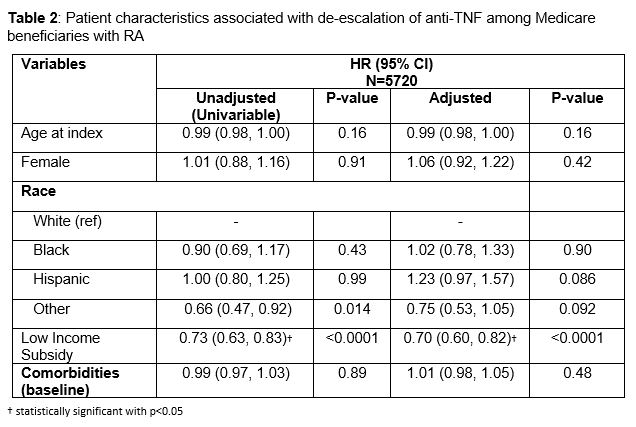
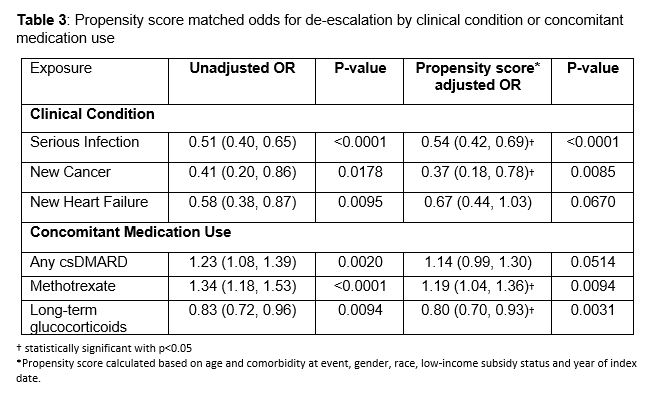
Methods: We identified adults ≥66 years of age with RA, on anti-TNF therapy within 6-months of RA diagnosis with at least 6-7 months duration (proxy for stable use), using 20% Medicare data from 2009-2017. Patient demographic and clinical characteristics including concomitant use of glucocorticoid (GC) and conventional synthetic DMARDs (csDMARDs) were collected. Anti-TNF use was categorized as either de-escalation, identified by dose reduction, dosing interval increase or cessation of use, or continuation. We used (1) prospective cohort design with Cox regression models to analyze the association between patient characteristics and time to de-escalation event and, (2) case-control design with propensity score adjusted logistic regression to retrospectively assess the association of de-escalation with different clinical conditions and concomitant medication use.
Results: We identified 5720 Medicare beneficiaries with RA on anti-TNF. Average age at index was 74.0 (SD 5.8), 78% were female, 83% were non-Hispanic white, 26% had low income subsidy (LIS), and average Elixhauser comorbidity score was 2.2 (SD 1.9). One in five (21%) met criteria for de-escalation, of whom 61% either reduced dose or increased dosing interval and 39% ceased use. De-escalation was less likely in those with LIS status (HR 0.70, 95% CI 0.60-0.82), adjusting for patient age, sex, race/ethnicity, and comorbidity. Lower odds of de-escalation was associated with serious infection (OR 0.54, 95% CI 0.42-0.69), new cancer diagnosis (OR 0.37, 95% CI 0.18-0.78), and long-term GC use (OR 0.80, 95% CI 0.70-0.93), whereas higher odds was associated with concomitant methotrexate use (OR 1.19, 95% CI 1.04-1.36).
Conclusion: Although older adults with greater burden of polypharmacy and multimorbidity are more likely to benefit from de-escalation, anti-TNFs are de-escalated in 21% of older adults with RA in usual care. This in comparison to clinical trials showing 30-50% of younger adults with RA can de-escalate bDMARDs without significant disease progression. Further study to understand sub-groups of older adults with RA most likely to benefit from and the impact of de-escalation can help optimize the use of anti-TNFs in this population.
To cite this abstract in AMA style:
Lee J, Kumar N, Kabeto M, Galecki A, Chang C, Singh N, Yung R, Makris U, Bynum J. De-escalation of Anti-TNFs in Older Adults with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/de-escalation-of-anti-tnfs-in-older-adults-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/de-escalation-of-anti-tnfs-in-older-adults-with-rheumatoid-arthritis/